Skin cancer
The primary cause of skin cancer is prolonged exposure to ultraviolet (UV) radiation from the sun or tanning devices.
[5][14] Basal-cell cancer grows slowly and can damage the tissue around it but is unlikely to spread to distant areas or result in death.
[3] Decreasing exposure to ultraviolet radiation and the use of sunscreen appear to be effective methods of preventing melanoma and squamous-cell skin cancer.
[5] Treatment is generally by surgical removal but may, less commonly, involve radiation therapy or topical medications such as fluorouracil.
[3] In those people whose disease has spread to other areas of the body, palliative care may be used to improve quality of life.
[6][22] The three main types of skin cancer have become more common in the last 20 to 40 years, especially regions where the population is predominantly White.
BCC and SCC often carry a UV-signature mutation indicating that these cancers are caused by UVB radiation via direct DNA damage.
Other common signs of skin cancer can be painful lesion that itches or burns and large brownish spot with darker speckles.
Warning signs of malignant melanoma include change in the size, shape, color or elevation of a mole.
An often-used mnemonic is "ABCDE", where A is for "asymmetrical", B for "borders" (irregular: "Coast of Maine sign"), C for "color" (variegated), D for "diameter" (larger than 6 mm – the size of a pencil eraser) and E for "evolving.
"[26][27] Merkel cell carcinomas are most often rapidly growing, non-tender red, purple or skin colored bumps that are not painful or itchy.
Other risk factors that play a role include: UV-irradiation of skin cells causes damage to DNA through photochemical reactions.
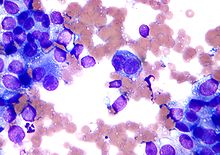
Microscopically, tumor cells destroy the basement membrane and form sheets or compact masses which invade the subjacent connective tissue (dermis).
In well differentiated carcinomas, tumor cells are pleomorphic/atypical, but resembling normal keratinocytes from prickle layer (large, polygonal, with abundant eosinophilic (pink) cytoplasm and central nucleus).
[39] Their disposal tends to be similar to that of normal epidermis: immature/basal cells at the periphery, becoming more mature to the centre of the tumor masses.
[39] A molecular factor involved in the disease process is mutation in gene PTCH1 that plays an important role in the Sonic hedgehog signaling pathway.
[42] There is insufficient evidence that optical coherence tomography (OCT) is useful in diagnosing melanoma or squamous cell carcinoma.
[43] Computer-assisted diagnosis devices have been developed that analyze images from a dermatoscope or spectroscopy and can be used by a diagnostician to aid in the detection of skin cancer.
[50] The U.S. Preventive Services Task Force recommends that people between 9 and 25 years of age be advised to avoid ultraviolet light.
It is important to limit sun exposure and to avoid tanning beds, because they both involve UV light.
[57] A meta-analysis of skin cancer prevention in high risk individuals found evidence that topical application of T4N5 liposome lotion reduced the rate of appearance of basal cell carcinomas in people with xeroderma pigmentosum, and that acitretin taken by mouth may have a skin protective benefit in people following kidney transplant.
For a small basal-cell cancer in a young person, the treatment with the best cure rate (Mohs surgery or CCPDMA) might be indicated.
In the case of an elderly frail man with multiple complicating medical problems, a difficult to excise basal-cell cancer of the nose might warrant radiation therapy (slightly lower cure rate) or no treatment at all.
Additionally, scientists are testing a vaccine designed to match the unique genetic details of a patient's cancer in an advanced clinical trial.
Excision and reconstruction of facial skin cancers are generally more challenging due to the presence of highly visible and functional anatomic structures in the face.
If the repair is made along a natural skin fold or wrinkle line, the scar will be hardly visible.
Various forms of local flaps can be designed to minimize disruption to surrounding tissues and maximize cosmetic outcome of the reconstruction.
Once the flap develops a source of blood supply form its new bed, the vascular pedicle can be detached.
The cure rate is very high when melanoma is detected in early stages, when it can easily be removed surgically.
[69] As of 2003 the overall five-year cure rate with Mohs' micrographic surgery was around 95 percent for recurrent basal cell carcinoma.



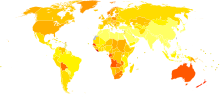
|
no data
<0.7
0.7–1.4
1.4–2.1
2.1–2.8
2.8–3.5
3.5–4.2
|
4.2–4.9
4.9–5.6
5.6–6.3
6.3–7
7–7.7
>7.7
|