Social determinants of health in poverty
[1] Poverty has many dimensions – material deprivation (of food, shelter, sanitation, and safe drinking water), social exclusion, lack of education, unemployment, and low income – that all work together to reduce opportunities, limit choices, undermine hope, and, as a result, threaten health.
[2] Poverty has been linked to higher prevalence of many health conditions, including increased risk of chronic disease, injury, deprived infant development, stress, anxiety, depression, and premature death.
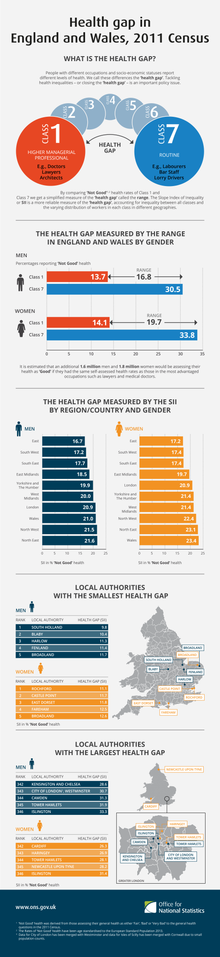
Socioeconomic factors that affect impoverished populations such as education, income inequality, and occupation, represent the strongest and most consistent predictors of health and mortality.
[1] The inequitable distribution of health-harmful living conditions, experiences, and structures, is not by any means natural, "but is the result of a toxic combination of poor social policies and programmes, unfair economic arrangements, and bad politics".
[1] Along with these social conditions, "Gender, education, occupation, income, ethnicity, and place of residence are all closely linked to people's access to, experiences of, and benefits from health care.
Structural determinants include societal divisions between social, economic, and political contexts, and lead to differences in power, status, and privilege within society.
Absolute poverty is the severe deprivation of basic human needs such as food, safe drinking water and shelter, and is used as a minimum standard below which no one should fall regardless of where they live.
[11] Having sufficient access to a minimum amount of food that is nutritious and sanitary plays an important part in building health and reducing disease transmission.
[11]Housing, including size, quality, ventilation, crowding, sanitation, and separation, prove paramount in determining health and spread of disease.
[1] The way in which resources such as income, nourishment, and emotional support are traded in the household influences women's psychosocial health, nutrition, wellness, access to healthcare services, and threat of violence.
[11] Health-related behaviors, access and use of healthcare, stress, and psychosocial resources like social ties, coping, and spirituality all serve as factors that mediate health inequality.
[10] Components of the geopolitical system that spawn gender and economic inequality, such as history of a nation, geography, policy, services, legal rights, organizations, institutions, and social structures, are all determinants of women's health in poverty.
[10] Evidence suggests that excess male mortality correlates with behavior considered socially acceptable among men, including smoking, binge drinking, and risky activities.
[24] Higher rates of chronic diseases[25] such as obesity and diabetes, as well as cigarette smoking[26] were found in adolescents aged 10–21 belonging to low socioeconomic status.
[30] African Americans, even in some of the wealthiest cities in the United States, have lower life expectancy at birth than people in much poorer countries like China or India.
[32] Farmer says the growing mortality differentials between whites and blacks must be attributed to class differentials-[30] which includes recognizing race within impoverished populations.
The CDC points to discrimination within health care, education, criminal justice, housing, and finance, direct results of systematically subversive tactics like redlining which led to chronic and toxic stress that shaped social and economic factors for minority groups, increasing their risk for COVID-19.
Healthcare access is similarly limited by factors like a lack of public transportation, child care, and communication and language barriers which result from the spatial and economic isolation of minority communities from redlining.
Educational, income, and wealth gaps that result from this isolation mean that minority groups' limited access to the job market may force them to remain in fields that have a higher risk of exposure to the virus, without options to take time off.
Finally, a direct result of redlining is the overcrowding of minority groups into neighborhoods that do not boast adequate housing to sustain burgeoning populations, leading to crowded conditions that make prevention strategies for COVID-19 nearly impossible to implement.
[42][43] Additionally, residents of impoverished communities are at increased risk for mental illness, chronic disease, higher mortality, and lower life expectancy.
[50] As one's job or career is a primary conduit for both financial and social capital, work is an important, yet under represented, factor in health inequities research and prevention efforts.
[10] Studies in the United States suggest maternal education results in higher parity, greater use of prenatal care, and lower smoking rates, which positively affects child health.
[1] The growing power of massive, conglomerate global corporations and institutions to set labor policy and standards agendas has disempowered workers, unions, and the job-seeking by subjecting these individuals to health-damaging working conditions.
Migrants have a variety of physical and mental health needs, shaped by their background, the host country's entry and integration policies, and their living and working conditions.
[1] In the 19th and 20th century, slums developed in cities and the ensuing crowding, poor sanitation, and inadequate dwellings brought infectious disease and illnesses, causing public health concerns.
Urban areas present health risks through poor living conditions, limited food resources, traffic accidents, and pollution.
[71] It pairs up senior volunteers with patients who come from low-income background to help them increase their social capability, ability to live independently and more accessibility to healthcare.
[73] The result is homogeneous with conclusions from other studies, with emerging themes include: companionship, reduced depression, access to healthcare, isolation, and increased social network.
Despite the strength of political influences, it has been shown that, globally, shifting attention to addressing social needs like healthcare access has dramatically affected the health of impoverished communities.