Spasmodic torticollis
Spasmodic torticollis is an extremely painful chronic neurological movement disorder causing the neck to involuntarily turn to the left, right, upwards, and/or downwards.
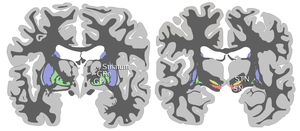
[4] Studies have suggested that there is a functional imbalance in the striatal control of the globus pallidus, specifically the substantia nigra pars reticulata.
[citation needed] Spasmodic torticollis is a form of focal dystonia, a neuromuscular disorder that consists of sustained muscle contractions causing repetitive and twisting movements and abnormal postures in a single body region.
[citation needed] Primary spasmodic torticollis is defined as having no other abnormality other than dystonic movement and occasional tremor in the neck.
[10] There are several treatments for spasmodic torticollis, the most commonly used being botulinum toxin injections in the dystonic muscle of the neck.
Other treatments include sensory trick for a mild occasional twinge, oral medications, and deep brain stimulation.
[7] In addition, selective surgical denervation of nerves triggering muscle contractions may offer relief from spasms and pain, and limit damage to the spine as a result of torqued posture.
[7] Since the root of the problem is neurological, doctors have explored sensorimotor retraining activities to enable the brain to "rewire" itself and eliminate dystonic movements.
Side effects include dry mouth, cognitive disturbance, drowsiness, diplopia, glaucoma and urinary retention.
Botulinum toxin type A is most often used; it prevents the release of acetylcholine from the presynaptic axon of the motor end plate, paralyzing the dystonic muscle.
[16] A Cochrane review published in 2016 reported moderate-quality evidence that a single Botulinum toxin-B treatment session could improve cervical dystonia symptoms by 10% to 20%, although with an increased risk of dry mouth and swallowing difficulties.
[23] Deep brain stimulation to the basal ganglia and thalamus has recently been used as a successful treatment for tremors of patients with Parkinson's disease.
The device is analogous to a pacemaker: an external battery is placed subcutaneously, with wires under the skin which enter the skull and a region of the brain.
Globus pallidus internus deep brain stimulation is the preferred surgical procedure, due to the lower frequency of side effects.
[17] In one study, patients who had developed immunoresistance to botulinum toxin underwent globus pallidus internus deep brain stimulation, showing improvement by 54.4% after three to six months.
[16] Physical treatment options for cervical dystonia include biofeedback, mechanical braces as well as patients self-performing a geste antagoniste.
Physical therapy also has an important role in managing spasmodic torticollis by providing stretching and strengthening exercises to aid the patient in keeping their head in proper alignment with their body.
A significant reduction in pain and severity of dystonia as well as increased postural awareness and quality of life was found.
[26] Spasmodic torticollis is one of the most common forms of dystonia seen in neurology clinics, occurring in approximately 0.390% of the United States population in 2007 (390 per 100,000).
[28] The exact prevalence of the disorder is not known; several family and population studies show that as many as 25% of cervical dystonia patients have relatives that are undiagnosed.