Stroke
[7] Other risk factors include high blood cholesterol, tobacco smoking, obesity, diabetes mellitus, a previous TIA, end-stage kidney disease, and atrial fibrillation.
[9] Prevention includes decreasing risk factors, surgery to open up the arteries to the brain in those with problematic carotid narrowing, and anticoagulant medication in people with atrial fibrillation.
These symptoms may include dizziness, dysarthria (speech disorder), exhaustion, hemiparesis (weakness on one side of the body), paresthesia (tingling, pricking, chilling, burning, numbness of the skin), pathological laughter, seizure that turns into paralysis, "thunderclap" headache, or vomiting.
A scoring system called ROSIER (recognition of stroke in the emergency room) is recommended for this purpose; it is based on features from the medical history and physical examination.
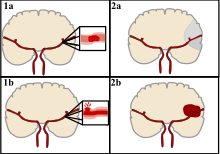
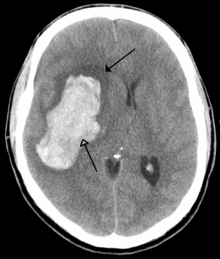
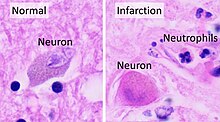
[43][44] Loss of consciousness, headache, and vomiting usually occur more often in hemorrhagic stroke than in thrombosis because of the increased intracranial pressure from the leaking blood compressing the brain.
A brainstem stroke affecting the brainstem and brain, therefore, can produce symptoms relating to deficits in these cranial nerves:[citation needed] If the cerebral cortex is involved, the central nervous system pathways can again be affected, but can also produce the following symptoms: If the cerebellum is involved, ataxia might be present and this includes: In the days before a stroke (generally in the previous 7 days, even the previous one), a considerable proportion of patients have a "sentinel headache": a severe and unusual headache that indicates a problem.
Because the reduction in blood flow is global, all parts of the brain may be affected, especially vulnerable "watershed" areas—border zone regions supplied by the major cerebral arteries.
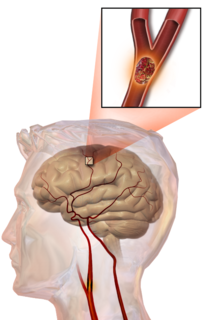
[67] Embolic infarction occurs when emboli formed elsewhere in the circulatory system, typically in the heart as a consequence of atrial fibrillation, or in the carotid arteries, break off, enter the cerebral circulation, then lodge in and block brain blood vessels.
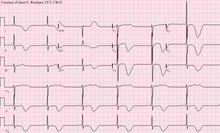
A physical examination, including taking a medical history of the symptoms and a neurological status, helps giving an evaluation of the location and severity of stroke.
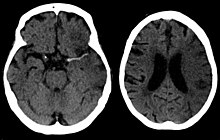
CT scans may not detect ischemic stroke, especially if it is small, of recent onset,[10] or in the brainstem or cerebellum areas (posterior circulation infarct).
[81] However, in people with obstruction of the internal carotid artery of one side, the presence of leptomeningeal collateral circulation is associated with reduced cerebral reserve capacity.
If this too does not identify an underlying reason for the bleeding, invasive cerebral angiography could be performed but this requires access to the bloodstream with an intravascular catheter and can cause further stroke as well as complications at the insertion site and this investigation is therefore reserved for specific situations.
[100] Alcohol use could predispose to ischemic stroke, as well as intracerebral and subarachnoid hemorrhage via multiple mechanisms (for example, via hypertension, atrial fibrillation, rebound thrombocytosis and platelet aggregation and clotting disturbances).
[108] Nonetheless, given the large body of circumstantial evidence, best medical management for stroke includes advice on diet, exercise, smoking and alcohol use.
[115][116][117] The available evidence does not show large differences in stroke prevention between antihypertensive drugs—therefore, other factors such as protection against other forms of cardiovascular disease and cost should be considered.
[131][132] Oral anticoagulants, especially Xa (apixaban) and thrombin (dabigatran) inhibitors, have been shown to be superior to warfarin in stroke reduction and have a lower or similar bleeding risk in patients with atrial fibrillation.
[162] Thrombolysis, such as with recombinant tissue plasminogen activator (rtPA), in acute ischemic stroke, when given within three hours of symptom onset, results in an overall benefit of 10% with respect to living without disability.
[173] 6.4% of people with large stroke developed substantial brain bleeding as a complication from being given tPA thus part of the reason for increased short term mortality.
[174] The American Academy of Emergency Medicine had previously stated that objective evidence regarding the applicability of tPA for acute ischemic stroke was insufficient.
[175] In 2013 the American College of Emergency Medicine refuted this position,[176] acknowledging the body of evidence for the use of tPA in ischemic stroke;[177] but debate continues.
[178][179] Intra-arterial fibrinolysis, where a catheter is passed up an artery into the brain and the medication is injected at the site of thrombosis, has been found to improve outcomes in people with acute ischemic stroke.
It also aims to help the survivor understand and adapt to difficulties, prevent secondary complications, and educate family members to play a supporting role.
Validated instruments such as the Barthel scale may be used to assess the likelihood of a person who has had stroke being able to manage at home with or without support subsequent to discharge from a hospital.
[medical citation needed] However, some people have reported that they continue to improve for years, regaining and strengthening abilities like writing, walking, running, and talking.
The body of evidence is uncertain on the efficacy of cognitive rehabilitation for reducing the disabling effects of neglect and increasing independence remains unproven.
The latest evidence supports the short-term benefits of motor imagery (MI) on walking speed in individuals who have had stroke, in comparison to other therapies.
[215] There are inadequate data on the effect of virtual reality and interactive video gaming on gait speed, balance, participation and quality of life.
[253] In 1658, in his Apoplexia, Johann Jacob Wepfer (1620–1695) identified the cause of hemorrhagic stroke when he suggested that people who had died of apoplexy had bleeding in their brains.
[255] Its use is now discouraged by a number of neurology textbooks, reasoning that the connotation of fortuitousness carried by the word accident insufficiently highlights the modifiability of the underlying risk factors.
[261] As of 2017, angioplasty and stents were under preliminary clinical research to determine the possible therapeutic advantages of these procedures in comparison to therapy with statins, antithrombotics, or antihypertensive drugs.






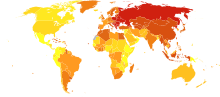

|
no data
<250
250–425
425–600
600–775
775–950
950–1125
|
1125–1300
1300–1475
1475–1650
1650–1825
1825–2000
>2000
|
