Thyroid nodule
Almost 50% of people have had one, but they are usually only detected by a physician during the course of a health examination or fortuitously discovered during the investigation of an unrelated condition.
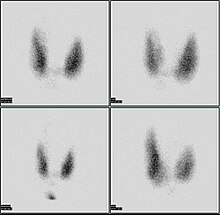
[8] The American College of Radiology recommends the following workup for thyroid nodules as incidental imaging findings on CT, MRI or PET-CT:[9] Ultrasound imaging is useful as the first-line, non-invasive investigation in determining the size, texture, position, and vascularity of a nodule, accessing lymph nodes metastasis in the neck, and for guiding fine needle aspiration cytology (FNAC) or biopsy.
[12] It was first proposed by Horvath et al.,[13] based on the BI-RADS (Breast Imaging Reporting and Data System) concept.
[14] TI-RADS developed by the American College of Radiology (ACR) guides clinicians in deciding which nodules require FNAC and in planning follow-up.
However, increased calcitonin levels can also be attributable to smoking, chronic alcohol consumption, usage of proton pump inhibitors, and renal failure.
Trouble swallowing or speaking, swollen cervical lymph nodes or a firm, immobile nodule are more indicative of malignancy, whereas a family history of autoimmune disease or goiter, thyroid hormonal dysfunction or a soft, painful nodule are more indicative of benignancy.
Other associations with neoplastic nodules are family history of thyroid cancer and prior radiation to the head and neck.
Children living near the Chernobyl nuclear power plant during the catastrophe of 1986 experienced a 60-fold increase in the incidence of thyroid cancer.
Thyroid cancer arising in the background of radiation is often multifocal with a high incidence of lymph node metastasis and has a poor prognosis.
[30] Surgery (thyroidectomy) may be indicated in some instances: Non-surgical, minimally invasive ultrasound-guided techniques are used for the treatment of large, symptomatic nodules.
[32] Focused ultrasounds have been used to treat other benign tumors, such as breast fibroadenomas and fibroid disease in the uterus.
[citation needed] Levothyroxine (T4) is a prohormone that peripheral tissues convert to the primary active thyroid hormone, triiodothyronine (T3).
According to a 1993 article, such nodules need to be treated only if they become toxic; surgical excision (thyroidectomy), radioiodine therapy, or both may be used.