Hashimoto's thyroiditis
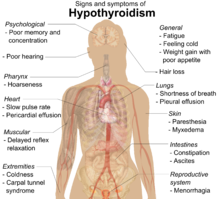
[3] Most people eventually develop hypothyroidism with accompanying weight gain, fatigue, constipation, hair loss, and general pains.
[15] While their role in the initial destruction of the follicles is unclear, antibodies against thyroid peroxidase or thyroglobulin are relevant, as they serve as biomarkers for detecting the disease and its severity.
[5] As lymphocytic infiltration progresses, patients may exhibit signs of hypothyroidism in multiple bodily systems, including, but not limited to, a larger goiter, weight gain, cold intolerance, fatigue, myxedema, constipation, menstrual disturbances, pale or dry skin, and dry, brittle hair, depression, and ataxia.
Symptoms can include: fatigue, weight gain, pale or puffy face, feeling cold, joint and muscle pain, constipation, dry and thinning hair, heavy menstrual flow or irregular periods, depression, a slowed heart rate, problems getting pregnant, miscarriages,[19] and myopathy.
[39] Development of Hashimoto's disease was associated with mutation of the gene for TNF-α (stimulator of the IFN-γ production), causing its higher concentration.
[40] Study of healthy Danish twins divided to three groups (monozygotic and dizygotic same sex, and opposite sex twin pairs) estimated that genetic contribution to thyroid peroxidase antibodies susceptibility was 61% in males and 72% in females, and contribution to thyroglobulin antibodies susceptibility was 39% in males and 75% in females.
[43] Another potential mechanism might be skewed X-chromosome inactivation,[5] leading to the escape of X-linked self-antigens from presentation in the thymus and loss of T-cell tolerance.
[citation needed] In one population study, two or more births were a risk factor for developing autoimmune hypothyroidism in pre-menopausal women.
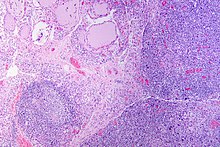
[58][59] Gross morphological changes within the thyroid are seen in the general enlargement, which is far more locally nodular and irregular than more diffuse patterns (such as that of hyperthyroidism).
While the capsule is intact and the gland itself is still distinct from surrounding tissue, microscopic examination can provide a more revealing indication of the level of damage.
[52] Key features detected in the ultrasound of a person with Hashimoto's thyroiditis include "echogenicity, heterogeneity, hypervascularity, and presence of small cysts.
[68] LC-MSMS assays are rarer, but they are "highly specific, sensitive, precise, and can detect hormones found in low concentrations.
[73] Levothyroxine has the benefits of a long half-life[23] leading to stable thyroid hormone levels,[74] ease of monitoring,[74] excellent safety[74][75] and efficacy record,[68] and usefulness in pregnancy as it can cross the fetal blood-brain barrier.
[15] Levothyroxine dosing to normalise TSH is based on the amount of residual endogenous thyroid function and the patient’s weight, particularly lean body mass.
"[21] Symptoms to watch for include, but are not limited to, anxiety, tremor, weight loss, heat sensitivity, diarrhea, and shortness of breath.
[71] The target level for TSH is the subject of debate, with factors like age, sex, individual needs and special circumstances such as pregnancy being considered.
[5] Measuring reverse tri-iodothyronine (rT3) is often mentioned in the lay (non-medical) press as a possible marker to inform T4 or T3 therapy, "however, there is currently no evidence to support this application" as of 2023.
[69] Although cited in the lay press as a possible competitor to T3, it is unlikely that rT3 causes hypothyroid symptoms by out-competing T3 for thyroid hormone receptors, as it has a binding affinity 200 times weaker.
[79][98][23] Hypothesised mechanisms include the proposal that TPO-antibody-producing lymphocytes may travel out of the thyroid to other tissue, creating symptoms and inflammation due to cross-reaction,[23][99] or "the inflammatory nature of [...] persistently increased circulating cytokine levels.
There is preliminary evidence that levothyroxine,[105][106] [needs update]aloe vera juice[107] and black cumin seed[108] may reduce thyroid peroxidase antibodies.
[109] One study found surgical thyroid removal can substantially reduce anti-thyroid antibody levels,[79][5] see Surgery considerations[clarification needed].
[5] Patients generally may discuss surgery with their doctor if they are experiencing significant pressure symptoms, or cosmetic concerns, or have nodules present on ultrasound.
[5] One well-conducted study of patients with troublesome general symptoms and with anti-thyroperoxidase (anti-TPO) levels greater than 1000 IU/ml (normal <100 IU/ml) showed that total thyroidectomy caused the symptoms to resolve and median anti-thyroid peroxidase levels to reduce from 2232 to 152 IU/mL,[5][110] but post-operative complications were higher than expected:[79] infection (4.1%), permanent hypoparathyroidism (4.1%) and recurrent laryngeal nerve injury (5.5%).
Transient periods of thyrotoxicosis (over-activity of the thyroid) sometimes occur, and rarely the illness may progress to full hyperthyroid Graves' disease with active orbitopathy (bulging, inflamed eyes).
Iodine levels in both water and salt should be heavily monitored in order to protect at-risk populations from developing hypothyroidism.
[60] It has been shown that the prevalence of positive tests for thyroid antibodies increases with age, "with a frequency as high as 33 percent in women 70 years old or older.
[4] Later on in the same year, researchers from the Middlesex Hospital in London were able to perform human experiments on patients who presented with similar symptoms.
[15] Levothyroxine treatment in euthyroid women with thyroid autoimmunity does not significantly impact the relative risk of miscarriage and preterm delivery, or outcomes with live birth.
[138] Several years after the delivery, the chimeric male cells can be detected in the maternal peripheral blood, thyroid, lung, skin, or lymph nodes.
In Hashimoto's disease patients, fetal microchimeric cells were detected in thyroid in significantly higher numbers than in healthy females.