Transcranial magnetic stimulation
[1]: 3 [2] TMS has shown diagnostic and therapeutic potential in the central nervous system with a wide variety of disease states in neurology and mental health, but has not demonstrated clinical worth for treatment of any other condition.
[7] TMS can be used clinically to measure activity and function of specific brain circuits in humans, most commonly with single or paired magnetic pulses.
[4] During the procedure, a magnetic coil is positioned at the head of the person receiving the treatment using anatomical landmarks on the skull, in particular the inion and nasion.
[19] Directing the magnetic field pulse at a targeted area in the brain causes a localized electrical current which can then either depolarize or hyperpolarize neurons at that site.
[20] Deep TMS can reach up to 6 cm into the brain to stimulate deeper layers of the motor cortex, such as that which controls leg motion.
The path of this current can be difficult to model because the brain is irregularly shaped with variable internal density and water content, leading to a nonuniform magnetic field strength and conduction throughout its tissues.
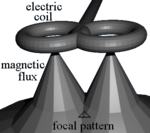
[21] The effects of TMS can be divided based on frequency, duration and intensity (amplitude) of stimulation:[22] Most devices use a coil shaped like a figure-eight to deliver a shallow magnetic field that affects more superficial neurons in the brain.
[29] The Hesed (H-core), circular crown and double cone coils allow more widespread activation and a deeper magnetic penetration.
They are supposed to impact deeper areas in the motor cortex and cerebellum controlling the legs and pelvic floor, for example, though the increased depth comes at the cost of a less focused magnetic pulse.
[30][31] Luigi Galvani (1737–1798) undertook research on the effects of electricity on the body in the late-eighteenth century and laid the foundations for the field of electrophysiology.
[33] Work to directly stimulate the human brain with electricity started in the late 1800s, and by the 1930s the Italian physicians Cerletti and Bini had developed electroconvulsive therapy (ECT).
[37][38] In August 2018, the US Food and Drug Administration (US FDA) authorized the use of TMS developed by the Israeli company Brainsway in the treatment of obsessive–compulsive disorder (OCD).
Camilla Nord, head of the Mental Health Neuroscience Lab at the University of Cambridge said "The NHS has unfortunately been far behind the US and Canada on rTMS, which is at least as effective as antidepressants, if not more".
[54][55][56][57] In contrast, UnitedHealthcare issued a medical policy for TMS in 2013 that stated there is insufficient evidence that the procedure is beneficial for health outcomes in patients with depression.
[58] Other commercial insurance plans whose 2013 medical coverage policies stated that the role of TMS in the treatment of depression and other disorders had not been clearly established or remained investigational included Aetna, Cigna and Regence.