Neurostimulation
[1][2] A recent scientific review (2024) has identified relevant hypotheses on the cellular-level processes underlying non-invasive neurostimulation.
[3] Data analysis revealed that mitochondrial activity probably plays a central role in brain stimulation implemented by different approaches.
In addition, analysis of the mother-fetus neurocognitive model [4] provided insights into the conditions of natural neurostimulation of the fetal nervous system during pregnancy.
According to prof Barbara Jobst and colleagues, the most explored targets for scheduled stimulation are the anterior nucleus of the thalamus and the hippocampus.
[6] Moreover, the cluster headache (CH) can be treated by using a temporary stimulating electrode at sphenopalatine ganglion (SPG).
Medical Dr. Mehdi Ansarinia and colleagues reported pain relief within several minutes of stimulation in this method.
Also, TMS can be used to determine the contribution of cortical networks to specific cognitive functions by disrupting activity in the focal brain region.
Cochlear implants include several subsystem components from the external speech processor and radio frequency (RF) transmission link to the internal receiver, stimulator, and electrode arrays.
In 1961, a crude single electrode device was implanted in two deaf patients and useful hearing with electric stimulation was reported.
[25] In cochlear implants, the sound is picked up by a microphone and transmitted to the behind-the-ear external processor to be converted to the digital data.
By extracting the power and demodulating the data, electric current commands are sent to the cochlea to stimulate the auditory nerve through microelectrodes.
[28] The internal unit in the cochlear implants is an ASIC (application-specific integrated circuit) chip that is responsible to ensure safe and reliable electric stimulation.
The forward pathway recovers digital information from the RF signal which includes stimulation parameters and some handshaking bits to reduce the communication error.
[34][citation needed] LGN, which is located in the midbrain to relay signals from the retina to the visual cortex, is another potential area that can be used for stimulation.
[36] Today, modern pulse generators are programmed non-invasively by sophisticated computerized machines using RF, obtaining information about the patient's and device's status by telemetry.
The pacemaker circuitry includes sense amplifiers to detect the heart's intrinsic electrical signals, which are used to track heart activity, rate adaptive circuitry, which determine the need for increased or reduced pacing rate, a microprocessor, memory to store the parameters, telemetry control for communication protocol and power supplies to provide regulated voltage.
[citation needed] These cochlear implant electrodes are either straight or spiral such as Med-El Combi 40+ and Advanced Bionics Helix microelectrodes respectively.
[citation needed] On the other hand, planar stretchable microelectrode arrays are formed from flexible polymers, such as silicone, polyimide, and Parylene as candidates for retinal implants.
There are several requirements for DBS microelectrodes that include long lifetime without injury to the tissue or degradation of the electrodes, customized for different brain sites, long-term biocompatibility of the material, mechanically durable in order to reach the target without being damaged during handling by the implant surgeon, and finally uniformity of performance across the microelectrodes in a particular array.
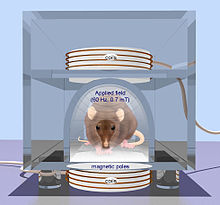
[40] While neurophysiology lacks knowledge about the nature of such a treatment of nervous diseases at the cellular level,[41] many non-invasive electrical and magnetic therapeutic methods involve excessive exposure of the patient to an intense field, which is several times and even orders of magnitude higher than natural currents and electromagnetic fields in the brain.
[42][43] Another significant challenge of non-invasive electrical and magnetic field methods is the impossibility of localizing the effect of stimulation on tissues in the relevant neural networks.
The relationship between neural activity and cognitive processes continues to be an intriguing research question and challenge for treatment selection.
[47] In the late 18th century, Luigi Galvani discovered that the muscles of dead frog legs twitched when struck by direct current on the nervous system.
[48] The modulation of the brain activity by electrical stimulation of the motor cortex in dogs was shown in 1870 that resulted in limb movement.
[52] A 2016 review of research on interactions between the nervous and immune systems in autoimmune disorders mentioned "electroceuticals" in passing and quotation marks, referring to neurostimulation devices in development for conditions like arthritis.
[53] In 2024, the introduction of the Mother-Fetus neurocognitive model and definition of the natural neurostimulation features revealed new perspectives to develop a novel generation of electroceutical medical devices.
[3] In addition to the enormous usage of neurostimulation for clinical applications, it is also used widely in laboratories started dates back to 1920s by people like Delgado who used stimulation as an experimental manipulation to study basics of how the brain works.
Another most recent example is the electrical stimulation of the middle temporal (MT) area of primary visual cortex to bias perception.
[citation needed] Generally, a short but high-frequency current in the range of 100 Hz helps strengthening the connection known as long-term potentiation.