Health insurance coverage in the United States
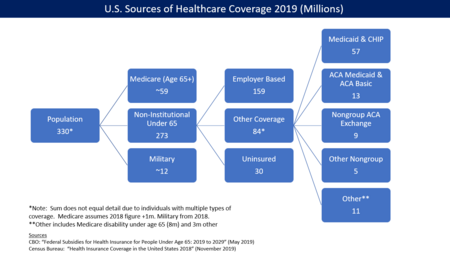
[1] For the 273 million non-institutional persons under age 65 in 2019:[1] The U.S. Centers for Disease Control and Prevention (CDC) reports the number and percentage of uninsured during each year.
The New York Times reported in January 2019 that the Trump Administration has taken a variety of steps to weaken the ACA, adversely affecting coverage.
[16] The increases in the number of uninsured in the first 3 years of the Trump administration (2017-2019) reversed in 2020–2021, as coronavirus relief measures expanded eligibility and reduced costs.
[10] Gallup estimated in July 2014 that the uninsured rate for adults (persons 18 years of age and over) was 13.4% as of Q2 2014, down from 18.0% in Q3 2013 when the health insurance exchanges created under the Patient Protection and Affordable Care Act (PPACA or "Obamacare") first opened.
[30] The study also found that 19% of U.S. adults surveyed reported serious problems paying medical bills, more than double the rate in the next highest country.
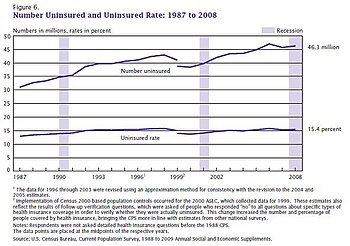
[32][33] The Independent reported that Families USA report "found that the spike in uninsured Americans – adding to an estimated 84 million people who are already uninsured or underinsured – is 39 per cent higher than any previous annual increase, including the most recent surge at the height of the recession between 2008 and 2009 when nearly 4 million non-elderly Americans lost insurance.
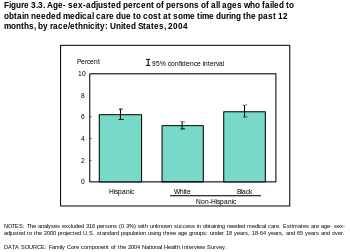
This is attributable to a higher likelihood of working in a low-wage job that does not offer health benefits, and restrictions on eligibility for public programs.
[41] A report by the Kaiser Family Foundation in April 2008 found that US economic downturns place a significant strain on state Medicaid and SCHIP programs.
[45] Critics of medical underwriting believe that it unfairly prevents people with relatively minor and treatable pre-existing conditions from obtaining health insurance.
[46] One large industry survey found that 13% of applicants for individual health insurance who went through medical underwriting were denied coverage in 2004.
This study did not distinguish between consumers who were quoted increased rates due to medical underwriting and those who qualified for standard or preferred premiums.
Beginning with wage and price controls during World War II, and cemented by an income tax exemption ruling in 1954, most working Americans have received their health insurance from their employers.
[55][56] Possible reasons include a lack of awareness of the programs or of how to enroll, reluctance due to a perceived stigma associated with public coverage, poor retention of enrollees, and burdensome administrative procedures.
[56] A study by the Kaiser Family Foundation published in June 2009 found that 45% of low-income adults under age 65 lack health insurance.
[59] City University public health professors David Himmelstein and Steffie Woolhandler wrote in January 2017 that a rollback of the ACA's Medicaid expansion alone would cause an estimated 43,956 deaths annually.
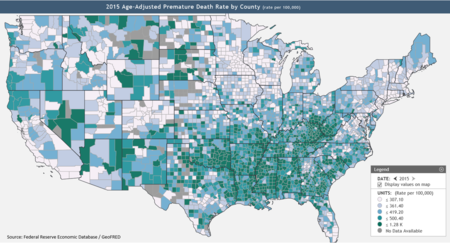
[62] Texas, Oklahoma, Mississippi, Alabama, Georgia, Tennessee, Missouri and South Carolina, indicated on the Federal Reserve map (see graph at right) as having many counties with high premature mortality rates,[58] did not expand Medicaid.
[69] A study found that in 2009, uninsured patients presenting in U.S. emergency departments were less likely to be admitted for inpatient care than those with Medicare, Medicaid, or private insurance.
section 1396r-4(g) governing hospital-specific limits on disproportionate share hospital payments under Title XIX of the Social Security Act.
Failure to act in the near term will only make it more expensive to cover the uninsured in the future, while adding to the amount of lost productivity from not insuring all Americans," said Professor Jack Hadley, the study's lead author.
[77] The reports concluded that the committee recommended that the nation should implement a strategy to achieve universal health insurance coverage.
The financial stability of a whole family can be put at risk if only one person is uninsured and needs treatment for unexpected health care costs.
This report recommended the following: The President and Congress need to develop a strategy to achieve universal insurance coverage and establish a firm schedule to reach this goal by the year 2010.
They also warned that the federal and state governments should prevent the erosion of outreach efforts, eligibility, enrollment, and coverage of these specific programs.
Adults who have cardiovascular disease or other cardiac risk factors that are uninsured are less likely to be aware of their condition, which leads to worse health outcomes for those individuals.
Without health insurance, adults are more likely to be diagnosed with certain cancers that would have been detectable earlier by screening by a clinician if they had regularly visited a doctor.
[86] In October 2020, Health Affairs writers summarized the results of several studies that placed the higher death rates for the uninsured between 1 per 278 to 1 per 830 persons without insurance: "Based on the ACS coverage data, we estimate that between 3,399 and 10,147 excess deaths among non-elderly US adults may have occurred over the 2017-2019 time period due to coverage losses during these years.
In 2020 and beyond, we can project even more loss of life if, as expected, millions more lose health coverage due to the economic downturn associated with the pandemic.
Indirect payments and reimbursements through federal and state government programs have never fully compensated public and private hospitals for the full cost of care mandated by EMTALA.
[7][89] People without health insurance in the United States may receive benefits from patient-assistance programs such as Partnership for Prescription Assistance.
On April 3, 2020, President Donald Trump announced that the federal government would use funds from the CARES Act to pay hospitals for treatment of uninsured patients infected with the virus that causes coronavirus disease 2019.