Vasodilation
[3] Relaxation of the smooth muscle layer allows the blood vessel to dilate, as it is held in a semi-constricted state by sympathetic nervous system activity.
Many of these substances are neurotransmitters released by perivascular nerves of the autonomic nervous system[6] Baroreceptors sense blood pressure and allow adaptation via the mechanisms of vasoconstriction or vasodilation to maintain homeostasis.
[8][9] Some physiologists have suggested that it is the lack of oxygen itself that causes capillary beds to vasodilate by the smooth muscle hypoxia of the vessels in the region.
Vasodilation occurs as part of the process of inflammation, which is caused by several factors including presence of a pathogen, injury to tissues or blood vessels, and immune complexes.
[7] Anti-inflammatory cytokines that regulate inflammation and help prevent negative results such as septic shock are also produced by these immune cells.
[7] Vasodilation and increased vascular permeability also allow immune effector cells to leave blood vessels and follow chemoattractants to the infection site via a process called leukocyte extravasation.
[4] Elevated vascular resistance due to constricted blood vessels causes in increase in afterload, the amount of force against which the heart must contract.
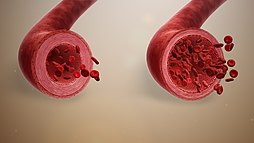
[16] Vasodilation works to decrease vascular resistance and blood pressure through relaxation of smooth muscle cells in the tunica media layer of large arteries and smaller arterioles.
Arterioles create the most vascular resistance of any blood vessel type, as they are very narrow and possess concentric layers of smooth muscle unlike venules and capillaries.
These processes are naturally modulated by local paracrine agents from endothelial cells (e.g., nitric oxide, bradykinin, potassium ions, and adenosine), and by the autonomic nervous system and the adrenal glands, both of which secrete catecholamines, such as norepinephrine and epinephrine, respectively.
[19][20] The tunica media of the walls of arteries, arterioles, and veins is composed of smooth muscle and causes vasodilation and vasoconstriction.
[21] Contraction is dependent on concentrations of Ca2+ in the cytosol, either via Ca,Mg-ATPase from the sarcoplasmic reticulum or voltage-gated calcium channels from the extracellular matrix.
[21] Phosphorylated light-chain myosin interacts with actin filaments forming a cross-bridge, allowing muscle contraction causing vasoconstriction.
[21] Smooth muscle cells can remain contracted without use of ATP due to action of the myosin-binding subunit of myosin light-chain phosphatase.
Phosphorylation of this subunit by Rho-kinase prevents it from binding to and dephosphorylating the myosin light-chain, allowing the cell to remain contracted.
This relaxation, in turn, relies on removing the stimulus for contraction, which depends on intracellular calcium ion concentrations and is tightly linked with phosphorylation of the light chain of the contractile protein myosin.
[2] Traditionally we understand that these two divisions work against each other, the SNS producing "fight or flight" and the PSNS producing "rest and digest", but in the case of vascular innervation this line becomes blurred[6] ANS nerves do not directly innervate the vasculature via synapses with muscle cells; instead, they release neurotransmitters that reach target cells and effect smooth muscle contraction or relaxation.
[2] SNS stimulation causes a base level of vasoconstriction often referred to as basal neural tone, maintaining blood pressure.
[28] It binds to α and β adrenergic receptors like norepinephrine, causing vasodilation and vasoconstriction in different body parts to redistribute circulation to critical areas.
Approximately five to ten minutes after the start of the cold exposure of the hand, the blood vessels in the finger tips will suddenly vasodilate.
This is probably caused by a sudden decrease in the release of neurotransmitters from the sympathetic nerves to the muscular coat of the arteriovenous anastomoses due to local cold.