Computed tomography of the abdomen and pelvis
Renal stones, appendicitis, pancreatitis, diverticulitis, abdominal aortic aneurysm, and bowel obstruction are conditions that are readily diagnosed and assessed with CT. CT is also the first line for detecting solid organ injury after trauma.
Multidetector CT (MDCT) can clearly delineate anatomic structures in the abdomen, which is critical in the diagnosis of internal diaphragmatic and other nonpalpable or unsuspected hernias.
[citation needed] In cases of suspected bowel leak or perforation, gastrointestinal fistula, interloop abscess or other fluid collection, oncologic staging and surveillance, and CT colonography, oral positive contrast is useful in delineating the lesions.
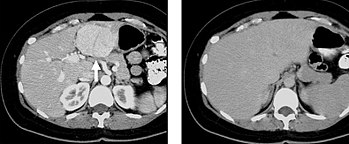
[citation needed] The most common technique is to perform portal venous phase imaging in the abdomen and pelvis (approximately 60–90 seconds after contrast administration, figure 2).
CTA is commonly used in the head and chest in the evaluation of pulmonary emboli, aneurysms, vascular malformations, dissection, bleeding and ischemia.
Although a "hypervascular", biphasic evaluation would generally be used for these patients, note that a single phase is often adequate for follow up imaging.
[citation needed] Delayed phase imaging (figure 5) encompasses scanning at a variety of different times following contrast administration, and depends on the pathology in question.
In addition, if there is a need to definitively characterize a hepatic mass, MRI is generally more sensitive and specific, with no associated radiation dose.
[citation needed] Transient hepatic attenuation differences in the arterial phase may mimic diseases of the liver.
Following noncontrast scanning, intravenous contrast is injected and a corticomedullary phase is obtained at approximately 70 seconds (figure 7a, 7b).
Excretory phase imaging allows for not only evaluation of the ureteral lumen, but also periureteral abnormalities including external masses and lymphadenopathy.
[citation needed] CT imaging should be performed to evaluate the specific clinical question, however incidental findings are noted in approximately 5-16 % of patients scanned for an unrelated reasons.
It is not acceptable practice to anticipate the possibility of incidental lesions given their low incidence and prospectively add additional phases to routine protocols.
Unfortunately, several recent surveys demonstrated that this practice is more common than might be anticipated, and contributes to unnecessary medical radiation exposure to a large population of patients.
A recent survey demonstrated that many physicians are routinely performing multiphase CT for the majority of patients in an attempt to prospectively characterize potential lesions detected during the scan.
However, unindicated multiphase CT examinations are an important source of medical radiation that does not contribute to the care of patients.
Adherence to published standards such as the ACR appropriateness criteria can both decrease medical radiation and optimize imaging for the specific clinical indication.