Angle-resolved low-coherence interferometry
Combining these techniques allows construction of a system that can measure average scatter size at various depths within a tissue sample.
At present the most significant medical application of the technology is determining the state of tissue health based on measurements of average cell nuclei size.
[1] Several recent studies[2] have shown that via cell nuclei measurements, a/LCI can detect the presence of low- and high-grade dysplasia with 91% sensitivity and distinguish between normal and dysplastic with 97% specificity.
[4] Variations in scattering distributions as a function of angle or wavelength have been used to deduce information regarding the size of cells and subcellular objects such as nuclei and organelles.
Light scattering spectroscopy has been used to detect dysplasia in the colon, bladder, cervix, and esophagus of human patients.
[5] However, in contrast with a/LCI, these techniques all rely on total intensity based measurements, which lack the ability to provide results as a function of depth in the tissue.
[7] This early system required up to 40 minutes to acquire the data for a 1 mm² point in a sample, but proved the feasibility of the idea.
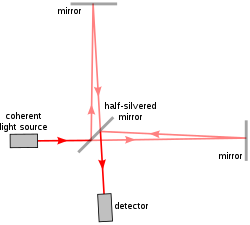
Like OCT, the early implementations of a/LCI relied on physically changing the optical path length (OPL) to control the depth in the sample from which data are acquired.
Finally the data is Fourier transformed on a line-by-line basis to generate scattering intensity as a function of OPL and angle.
Light from the sample and reference arms are mixed by a beamsplitting cube (BS), and are incident on the entrance slit of an imaging spectrometer.
Data from the imaging spectrometer are transferred to a computer via USB interface for signal processing and display of results.