Antipsychotic
[6][7] A recent controlled trial suggests that second generation antipsychotics[9] combined with intensive psychosocial therapy[10] may potentially prevent pallidal brain volume loss in first episode psychosis.
[11][8] The use of antipsychotics may result in many unwanted side effects such as involuntary movement disorders, gynecomastia, impotence, weight gain and metabolic syndrome.
[20] Aripiprazole, an atypical antipsychotic, is used as add-on medication to ameliorate sexual dysfunction as a symptom of selective serotonin reuptake inhibitor (SSRI) antidepressants in women.
Test results are combined with family history information to identify patients in the "high-risk" group; they are considered to have a 20–40% risk of progression to frank psychosis within two years.
The goals of continuing treatment are to maintain suppression of symptoms, prevent relapse, improve quality of life, and support engagement in psychosocial therapy.
[3][25] Maintenance therapy with antipsychotic drugs is clearly superior to placebo in preventing relapse but is associated with weight gain, movement disorders, and high dropout rates.
[40] A 3-year trial following persons receiving maintenance therapy after an acute psychotic episode found that 33% obtained long-lasting symptom reduction, 13% achieved remission, and only 27% experienced satisfactory quality of life.
Antipsychotics in long-acting injectable (LAI), or "depot", form have been suggested as a method of decreasing medication nonadherence (sometimes also called non-compliance).
A number of studies have looked at levels of "compliance" or "adherence" with antipsychotic regimes and found that discontinuation (stopping taking them) by patients is associated with higher rates of relapse, including hospitalization.
[60] Antipsychotics in old age dementia showed a modest benefit compared to placebo in managing aggression or psychosis, but this is combined with a fairly large increase in serious adverse events.
[72][73] Some of the more serious adverse effects may also occur at the low doses used, such as dyslipidemia and neutropenia,[74][75] and a recent network meta-analysis of 154 double-blind, randomized controlled trials of drug therapies vs. placebo for insomnia in adults found that quetiapine did not demonstrated any short-term benefits in sleep quality.
[77] Despite the lack of evidence supporting the benefit of antipsychotics in people with personality disorders, 1 in 4 who do not have a serious mental illness are prescribed them in UK primary care.
A recent randomized controlled trial, however, found no benefit over placebo and recommended that the use of antipsychotics in this way should no longer be regarded as an acceptable routine treatment.
[100][101][102] In contrast, other researchers point to the significantly higher risk of tardive dyskinesia and other extrapyramidal symptoms with the typicals and for this reason alone recommend first-line treatment with the atypicals, notwithstanding a greater propensity for metabolic adverse effects in the latter.
[104] Antipsychotics, such as risperidone, quetiapine, and olanzapine, have been used as hallucinogen antidotes or "trip killers" to block the effects of serotonergic psychedelics like psilocybin and lysergic acid diethylamide (LSD).
More serious adverse effects include seizures, NMS, neutropenia, and agranulocytosis (lowered white blood cell count) and its use needs careful monitoring.
[143] The National Association of State Mental Health Program Directors said that antipsychotics are not interchangeable, and it recommends including trying at least one weight-neutral treatment for those patients with potential metabolic issues.
[154] A randomised controlled trial compared maintenance therapy with gradual dose reduction or discontinuation among people with long-term psychosis.
[161] The British National Formulary recommends a gradual dose reduction when discontinuing antipsychotic treatment to avoid acute withdrawal symptoms or rapid relapse.
City and Hackney Clinical Commissioning Group found more than 1,000 patients in their area in July 2019 who had not had regular medication reviews or health checks because they were not registered as having serious mental illness.
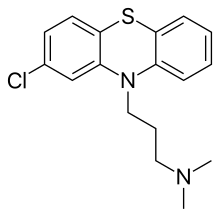
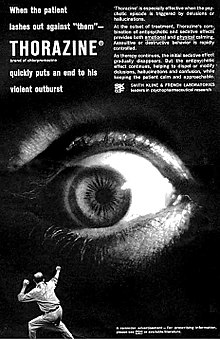
The discovery of chlorpromazine's psychoactive effects in 1952 led to further research that resulted in the development of antidepressants, anxiolytics, and the majority of other drugs now used in the management of psychiatric conditions.
[275] The term "ataraxy" was coined by the neurologist Howard Fabing and the classicist Alister Cameron to describe the observed effect of psychic indifference and detachment in patients treated with chlorpromazine.
[294] In case reports, quetiapine has been abused in doses taken by mouth (which is how the drug is available from the manufacturer), but also crushed and insufflated or mixed with water for injection into a vein.
[294] Joanna Moncrieff has argued that antipsychotic drug treatment is often undertaken as a means of control rather than to treat specific symptoms experienced by the patient.
[296] In an official review commissioned by UK government ministers it was reported that the needless use of antipsychotic medication in dementia care was widespread and was linked to 1800 deaths per year.
Following charges of illegal marketing, settlements by two large pharmaceutical companies in the US set records for the largest criminal fines ever imposed on corporations.
[300] In addition, AstraZeneca faces numerous personal-injury lawsuits from former users of Seroquel (quetiapine), amidst federal[clarification needed] investigations of its marketing practices.
[286] Harvard University medical professor Joseph Biederman conducted research on bipolar disorder in children that led to an increase in such diagnoses.
investigation found that Biederman also received $1.6 million in speaking and consulting fees between 2000 and 2007, some of them undisclosed to Harvard, from companies including makers of antipsychotic drugs prescribed for children with bipolar disorder.
[303] Physicians and caretakers of persons with dementia should try to address symptoms including agitation, aggression, apathy, anxiety, depression, irritability, and psychosis with alternative treatments whenever antipsychotic use can be replaced or reduced.