Artificial insemination
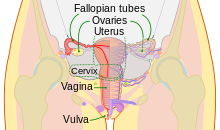
Artificial insemination is the deliberate introduction of sperm into a female's cervix or uterine cavity for the purpose of achieving a pregnancy through in vivo fertilization by means other than sexual intercourse.
[6] In the United Kingdom, the British obstetrician Mary Barton founded one of the first fertility clinics to offer donor insemination in the 1930s, with her husband Bertold Wiesner fathering hundreds of offspring.
[7][8] In the 1980s, direct intraperitoneal insemination (DIPI) was occasionally used, where doctors injected sperm into the lower abdomen through a surgical hole or incision, with the intention of letting them find the oocyte at the ovary or after entering the genital tract through the ostium of the fallopian tube.
It is painless and is the simplest, easiest and most common method of artificial insemination involving the introduction of unwashed or raw semen into the vagina at the entrance to the cervix, usually by means of a needleless syringe.
It is important that the syringe is emptied slowly for safety and for the best results, bearing in mind that the purpose of the procedure is to replicate as closely as possible a natural deposit of the semen in the vagina.
It is therefore the method of choice for single and lesbian women wishing to conceive using donor sperm since this group of recipients usually require artificial insemination because they do not have a male partner, not because they have medical problems.
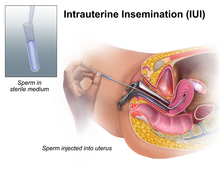
Owing to the high number of these recipients using donor sperm services, IUI is therefore the most popular method of insemination today at a fertility clinic.
For heterosexual couples, the indications to perform an intrauterine insemination are usually a moderate male factor, the incapability to ejaculate in vagina and an idiopathic infertility.
Lesbians and single women are less likely to have fertility issues of their own and enabling donor sperm to be inserted directly into the womb will often produce a better chance of conceiving.
A female under 30 years of age has optimal chances with IUI; A promising cycle is one that offers two follicles measuring more than 16 mm, and estrogen of more than 500 pg/mL on the day of hCG administration.
[19] However, GnRH agonist administration at the time of implantation does not improve pregnancy outcome in intrauterine insemination cycles according to a randomized controlled trial.
[28] Due to the lack of reliable evidence from controlled clinical trials, it is not certain which semen preparation techniques are more effective (wash and centrifugation; swim-up; or gradient) in terms of pregnancy and live birth rates.
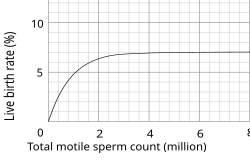
[30] Along with age, the duration of fertility is also found to be a factor in IUI success, the longer one faces infertility, the lower the chance of a positive pregnancy test occurring.
[30] When people talk about age as a risk factor, they are generally speaking to the way in which the DNA in the eggs and sperm have increased probabilities of mutations.
[30] The number of follicles developed, grown, and retrieved from the ovaries during ovarian stimulation is particularly important and a major success factor in fertility treatments.
[30] IUI can additionally be a good fertility outlet for lesbian or queer couples as they most often do not face infertility, and would most likely be using regulated and checked donor sperm.
[32] Intratubal insemination (ITI) involves injection of washed sperm into the fallopian tube, although this procedure is no longer generally regarded as having any beneficial effect compared with IUI.
[33] ITI however, should not be confused with gamete intrafallopian transfer, where both eggs and sperm are mixed outside the woman's body and then immediately inserted into the fallopian tube where fertilization takes place.
Although many fertilization procedures, such as IUI are typically carried out in a medical setting, society is increasingly recognizing the important role that this plays in the lives of individuals who might otherwise not conceive through heterosexual penetrative sexual intercourse.
While clinic based IUI may be open to many, it typically still includes hetero-reproductive narratives which dates from the early days of fertilization procedures when these were often exclusively for married couples and when there was a resistance in many societies to extend these services to the LGBTQ+ community.
One of the key issues arising from the rise of dependency on assisted reproductive technology (ARTs) is the pressure placed on couples to conceive, "where children are highly desired, parenthood is culturally mandatory, and childlessness socially unacceptable".
For instance, it was found that LGBTQ+ individuals had "had significant knowledge gaps of risk factors associated with reproductive outcomes when compared to heterosexual female peers.
[55] Under the 1973 UPA, married heterosexual couples making use of artificial insemination through a licensed physician could list the husband as the natural father of the child, rather than the sperm donor.
[55] Since then a revised version of the Act has been introduced, though to less widespread adoption[55] Generally paternity is not an issue when artificial insemination is between a married woman and an anonymous donor.
However, according to a document of the USCCB, the intrauterine insemination (IUI) of “licitly obtained” (normal intercourse with a silastic sheath i.e. a perforated condom) but technologically prepared semen sample (washed, etc.)
[56] Some religious groups, such as the Catholic Church, and individuals have also criticized artificial insemination because acquiring sperm for the procedure is seen as "a form of adultery promoting the vice of masturbation.
The line of reasoning follows the history of artificial insemination in breeding livestock and other domesticated animals wherein preferred traits are encouraged through human-controlled selection.
He improved breeding efficiency by the use of antibiotics (first proven with penicillin in 1946) to control bacterial growth, decreasing embryonic mortality, and increase fertility.
This, and various new techniques for processing, freezing, and thawing of frozen semen significantly enhanced the practical utilization of artificial insemination in the livestock industry and earned him the 1981 Wolf Foundation Prize in Agriculture.
In 2013 scientist of the Justus-Liebig-University of Giessen, Germany, from the working group of Michael Lierz, Clinic for birds, reptiles, amphibians, and fish, developed a novel technique for semen collection and artificial insemination in parrots producing the world's first macaw by assisted reproduction.