Asepsis
[1] Ideally, a surgical field is sterile, meaning it is free of all biological contaminants (e.g. fungi, bacteria, viruses), not just those that can cause disease, putrefaction, or fermentation.
The term often refers to those practices used to promote or induce asepsis in an operative field of surgery or medicine to prevent infection.
[8] Rubber gloves were pioneered by William Halsted, who also implemented a no street clothes policy in his operating room, opting to wear a completely white, sterile uniform consisting of a duck suit, tennis shoes, and skullcap.
[2] In his department at Johns Hopkins Hospital, he enforced an extreme hand washing ritual consisting of soaking in harmfully strong chemicals like permanganate and mercury bichloride solution as well as scrubbing with stiff brushes.
[6] Until the late 19th century, physicians rejected the connection between Louis Pasteur's germ theory that bacteria caused diseases and antiseptic techniques.
"[6] Generally, however, asepsis is seen as a continuation of antisepsis since many of the values are the same, such as a "germ-free environment around the wound or patient", and techniques pioneered under both names are used in conjunction today.
[15] Basic aseptic procedures includes hand washing, donning protective gloves, masks and gowns, and sterilizing equipment and linens.
[3] Tissue damage resulting from non-infectious means are caused by DAMPs molecules released after injury or cell death has occurred, which are able to stimulate inflammation response.
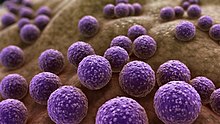
[19][20] The exact modes of infection depend on the types of surgery, but the most common bacteria that are responsible for SSIs are Staphylococcus aureus, coagulase-negative staphylococci, Escherichia coli, and Enterococcus spp.
[21] The CDC emphasizes the importance of both antiseptic and aseptic approaches in avoiding SSIs, especially since Staphylococcus aureus, among other bacteria, are able to evolve drug-resistant strains that can be difficult to treat.