Blood culture
Under normal conditions, the blood does not contain microorganisms: their presence can indicate a bloodstream infection such as bacteremia or fungemia, which in severe cases may result in sepsis.
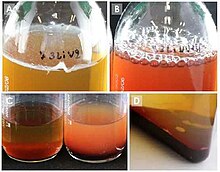
To perform the test, blood is drawn into bottles containing a liquid formula that enhances microbial growth, called a culture medium.
False negative results can occur if the sample is collected after the person has received antimicrobial drugs or if the bottles are not filled with the recommended amount of blood.
If microbial growth is detected, a Gram stain is conducted from the culture bottle to confirm that organisms are present and provide preliminary information about their identity.
The blood is then subcultured, meaning it is streaked onto an agar plate to isolate microbial colonies for full identification and antimicrobial susceptibility testing.
Because it is essential that bloodstream infections are diagnosed and treated quickly, rapid testing methods have been developed using technologies like polymerase chain reaction and MALDI-TOF MS.
[2] If bacteria or fungi are not cleared from the bloodstream, they can spread to other organs and tissues,[3] or evoke an immune response that leads to a systemic inflammatory condition called sepsis, which can be life-threatening.
[13][14][15] Bacteremia is common in some types of infections, such as meningitis, septic arthritis and epidural abscesses, so blood cultures are indicated in these conditions.
[11][19] The pathogens most frequently identified in blood cultures include Staphylococcus aureus, Escherichia coli and other members of the family Enterobacteriaceae, Enterococcus species, Pseudomonas aeruginosa and Candida albicans.
[20][21] Coagulase-negative staphylococci (CNS) are also commonly encountered, although it is often unclear whether these organisms, which constitute part of the normal skin flora,[22] are true pathogens or merely contaminants.
[11] Bottles intended for paediatric use are designed to accommodate lower blood volumes and have additives that enhance the growth of pathogens more commonly found in children.
Some manual blood culture systems indicate growth using a compartment that fills with fluid when gases are produced, or a miniature agar plate which is periodically inoculated by tipping the bottle.
[46] To ensure that positive blood cultures are not missed, a sample from the bottle is often inoculated onto an agar plate (subcultured) at the end of the incubation period regardless of whether or not indicators of growth are observed.
While lysis-centrifugation offers greater sensitivity than conventional blood culture methods, it is prone to contamination because it requires extensive manipulation of the sample.
[59] The Gram stain provides information about the possible identity of the organism, which assists the clinician in the selection of a more appropriate antimicrobial treatment before the full culture and sensitivity results are complete.
Positive bottles with negative Gram stains are subcultured before being returned to the incubator, often using special culture media that promotes the growth of slow-growing organisms.
[57] At this point, the microbiologist will assess the appearance of the bacterial or fungal colonies[62] and carry out tests that provide information about the metabolic and biochemical features of the organism, which permit identification to the genus or species level.
[29][64] Microorganisms may also be identified using automated systems, such as instruments that perform panels of biochemical tests,[65] or matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS), in which microbial proteins are ionized and characterized on the basis of their mass-to-charge ratios; each microbial species exhibits a characteristic pattern of proteins when analyzed through mass spectrometry.
[57] MALDI-TOF can be used to identify organisms directly from positive blood culture bottles after separation and concentration procedures,[68] or from preliminary growth on the agar plate within a few hours of subculturing.
[69] Genetic methods such as polymerase chain reaction (PCR) and microarrays can identify microorganisms by detection of DNA sequences specific to certain species in blood culture samples.
[42] It is also possible to directly inoculate microbial identification panels with blood from a positive culture bottle, although this is not as reliable as testing subcultured bacteria because additives from the growth media can interfere with the results.
[8][10] In traditional AST methods, such as the disk diffusion test, pure colonies of the organism are selected from the subculture plate and used to inoculate a secondary medium.
[65][75] Rapid administration of effective antimicrobial drugs is crucial in the treatment of sepsis,[8] so several methods have been developed to provide faster antibiotic sensitivity results.
[77][78] Because direct testing methods do not isolate the organisms, they do not provide accurate results if more than one microorganism is present, although this is an infrequent occurrence in blood cultures.
[87] A microbiology textbook from 1911 noted that decontamination of the draw site and equipment could take over an hour, and that due to a lack of effective methods for preserving blood, the cultures would sometimes have to be prepared at the patient's bedside.
Robert James Valentine Pulvertaft published a seminal work on blood cultures in 1930,[88] specifying—among other insights—an optimal blood-to-broth ratio of 1:5, which is still accepted today.
[86] From the 1940s through the 1980s, a great deal of research was carried out on broth formulations and additives, with the goal of creating a growth medium that could accommodate all common bloodstream pathogens.
[90] The earliest of these—the BACTEC systems, produced by Johnston Laboratories (now Becton Dickinson)—used culture broths containing nutrients labelled with radioactive isotopes.
[86] Throughout the 1970s and 80s several manufacturers attempted to detect microbial growth by measuring changes in the electrical conductivity of the culture medium, but none of these methods were commercially successful.
[93] The Difco ESP, a direct predecessor of the contemporary VersaTREK system[86] which detects gas production by measuring pressure changes, was also first approved in 1992.