Blunt trauma
Such incidents often occur with road traffic collisions, assaults, and sports-related injuries, and are notably common among the elderly who experience falls.
[1][2] Blunt trauma can lead to a wide range of injuries including contusions, concussions, abrasions, lacerations, internal or external hemorrhages, and bone fractures.
[3] Seventy-five percent of BAT occurs in motor vehicle crashes,[4] in which rapid deceleration may propel the driver into the steering wheel, dashboard, or seatbelt,[5] causing contusions in less serious cases, or rupture of internal organs from briefly increased intraluminal pressure in the more serious, depending on the force applied.
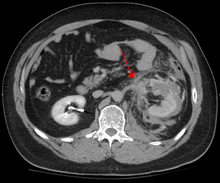
Initially, there may be few indications that serious internal abdominal injury has occurred, making assessment more challenging and requiring a high degree of clinical suspicion.
[8] In rare cases, this injury has been attributed to medical techniques such as the Heimlich maneuver,[9] attempts at CPR and manual thrusts to clear an airway.
Finally, the occurrence of splenic rupture with mild blunt abdominal trauma in those recovering from infectious mononucleosis or 'mono' (also known as 'glandular fever' in non-U.S. countries, specifically the UK) is well reported.
Common signs and symptoms include something as simple as bruising, but occasionally as complicated as hypoxia, ventilation-perfusion mismatch, hypovolemia, and reduced cardiac output due to the way the thoracic organs may have been affected.
Those experiencing more obvious complications from a blunt chest injury will likely undergo a focused assessment with sonography for trauma (FAST) which can reliably detect a significant amount of blood around the heart or in the lung by using a special machine that visualizes sound waves sent through the body.
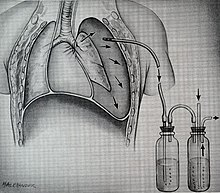
This tube is typically installed because it helps restore a certain balance in pressures (usually due to misplaced air or surrounding blood) that are impeding the lungs' ability to inflate and thus exchange vital gases that allow the body to function.
[16] The primary clinical concern with blunt trauma to the head is damage to the brain, although other structures, including the skull, face, orbits, and neck are also at risk.
[21] Vessels are examined for expanding hematoma, bruit, distal pulse exam, and signs/symptoms of ischemia, essentially asking, "Does blood seem to be getting through the injured area in a way that enough is getting to the parts past the injury?
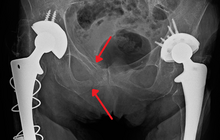
[24][25] Bones are evaluated with plain film X-ray or computed tomography if deformity (misshapen), bruising, or joint laxity (looser or more flexible than usual) are observed.
[27] In the pelvis specifically, the structures at risk include the pelvic bones, the proximal femur, major blood vessels such as the iliac arteries, the urinary tract, reproductive organs, and the rectum.
During the evaluation of trauma patients in an emergency department, the stability of the pelvis is typically assessed by the healthcare provider to determine whether a fracture may have occurred.
While BCIs necessitate a substantial amount of force to occur because the heart is well-protected by the rib cage and sternum, the majority of patients are asymptomatic.
In the US, the American College of Surgeons publishes the Advanced Trauma Life Support guidelines, which provide a step-by-step approach to the initial assessment, stabilization, diagnostic reasoning, and treatment of traumatic injuries that codifies this general principle.
The amount of time spent on diagnosis should be minimized and expedited by a combination of clinical assessment and appropriate use of technology,[33] such as diagnostic peritoneal lavage (DPL), or bedside ultrasound examination (FAST)[34] before proceeding to laparotomy if required.
Its disadvantages include the time taken to acquire images, although this gets shorter with each generation of scanners, and the removal of the patient from the immediate view of the emergency or surgical staff.
[36] When blunt trauma is significant enough to require evaluation by a healthcare provider, treatment is typically aimed at treating life-threatening injuries, such as maintaining the patient's airway and preventing ongoing blood loss.
[7] In these cases, it is essential to perform exploratory surgery to assess the internal damage, drain infected fluid in the abdomen, and clean the wound with saline.
[7] In the case of multiple holes or significant damage to the blood supply of the intestines, the affected segment of tissue may need to be removed entirely.
[17] Lastly, healthcare professionals should conduct consecutive neurological examinations to allow for early identification of elevated intracranial pressure and subsequent implementation of interventions to improve blood flow and reduce stress to the body.
Conservative measures such as maintaining a clear and open airway, oxygen support, tube thoracostomy, and volume resuscitation are often given to manage blunt thoracic trauma.
[37] Pain management in thoracic trauma patients improves the ability to breathe properly on their own, encourages the excretion of pulmonary secretions, and decreases the aggravation of inflammation and low oxygen levels in the blood.