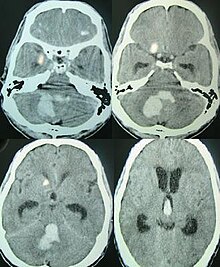
Intracerebral hemorrhage
[1] Treatment should typically be carried out in an intensive care unit due to strict blood pressure goals and frequent use of both pressors and antihypertensive agents.
[1] A procedure to place an external ventricular drain may be used to treat hydrocephalus or increased intracranial pressure, however, the use of corticosteroids is frequently avoided.
It is more likely to result in death or major disability than ischemic stroke or subarachnoid hemorrhage, and therefore constitutes an immediate medical emergency.
Intracerebral hemorrhages and accompanying edema may disrupt or compress adjacent brain tissue, leading to neurological dysfunction.
Substantial displacement of brain parenchyma may cause elevation of intracranial pressure (ICP) and potentially fatal herniation syndromes.
[7] While the duration of onset may not be as rapid, it is important that patients go to the emergency department as soon as they notice any symptoms as early detection and management of stroke may lead to better outcomes post-stroke than delayed identification.
Brain herniation is associated with hyperventilation, extensor rigidity, pupillary asymmetry, pyramidal signs, coma and death.
[10] Hemorrhage into the basal ganglia or thalamus causes contralateral hemiplegia due to damage to the internal capsule.
[7] Some cases of cerebellar hemorrhage lead to blockage of the fourth ventricle with subsequent impairment of drainage of cerebrospinal fluid from the brain.
[7] Cerebral amyloid angiopathy, a disease characterized by deposition of amyloid beta peptides in the walls of the small blood vessels of the brain, leading to weakened blood vessel walls and an increased risk of bleeding; is also an important risk factor for the development of intracerebral hemorrhage.
Other risk factors include advancing age (usually with a concomitant increase of cerebral amyloid angiopathy risk in the elderly), use of anticoagulants or antiplatelet medications, the presence of cerebral microbleeds, chronic kidney disease, and low low density lipoprotein (LDL) levels (usually below 70).
[12] So frequently, a CT angiogram will be performed in order to exclude a secondary cause of hemorrhage[30] or to detect a "spot sign".
[14] When due to high blood pressure, intracerebral hemorrhages typically occur in the putamen (50%) or thalamus (15%), cerebrum (10–20%), cerebellum (10–13%), pons (7–15%), or elsewhere in the brainstem (1–6%).
Rapid lowering of the blood pressure using antihypertensive therapy for those with hypertensive emergency can have higher functional recovery at 90 days post intracerebral haemorrhage, when compared to those who undergone other treatments such as mannitol administration, reversal of anticoagulation (those previously on anticoagulant treatment for other conditions), surgery to evacuate the haematoma, and standard rehabilitation care in hospital, while showing similar rate of death at 12%.
[43][44] Surgery is required if the hematoma is greater than 3 cm (1 in), if there is a structural vascular lesion or lobar hemorrhage in a young patient.
[34] A catheter may be passed into the brain vasculature to close off or dilate blood vessels, avoiding invasive surgical procedures.
[45] Aspiration by stereotactic surgery or endoscopic drainage may be used in basal ganglia hemorrhages, although successful reports are limited.
Rate of haematoma expansion, perihaematoma odema volume and the presence of fever can affect the chances of getting neurological complications.
[24] This kind of hemorrhage can also occur in the cortex or subcortical areas, usually in the frontal or temporal lobes when due to head injury, and sometimes in the cerebellum.
[7] Intraventricular hemorrhage, or bleeding into the ventricles of the brain, which may occur in 30–50% of patients, is also associated with long-term disability and a poor prognosis.
[51] Even though the majority of deaths occur in the first few days after ICH, survivors have a long-term excess mortality rate of 27% compared to the general population.
[52] Of those who survive an intracerebral hemorrhage, 12–39% are independent with regard to self-care; others are disabled to varying degrees and require supportive care.