Bulimia nervosa
[4] Other risk factors for the disease include psychological stress, cultural pressure to attain a certain body type, poor self-esteem, and obesity.
[4] Diagnosis is based on a person's medical history;[5] however, this is difficult, as people are usually secretive about their binge eating and purging habits.
[11][9] This cycle may be repeated several times a week or, in more serious cases, several times a day[12] and may directly cause: These are some of the many signs that may indicate whether someone has bulimia nervosa:[18] As with many psychiatric illnesses, delusions can occur, in conjunction with other signs and symptoms, leaving the person with a false belief that is not ordinarily accepted by others.
[20] People with bulimia exhibit several interoceptive deficits, in which one experiences impairment in recognizing and discriminating between internal sensations, feelings, and emotions.
One study found 70% had depression at some time in their lives (as opposed to 26% for adult females in the general population), rising to 88% for all affective disorders combined.
[25] Some individuals with anorexia nervosa exhibit episodes of bulimic tendencies through purging (either through self-induced vomiting or laxatives) as a way to quickly remove food in their system.
This can be caused by a childhood in which inner feelings and thoughts were minimized by parents, leading to "a high focus on receiving validation from others to maintain a positive sense of self".
[34] Scientific research has shown that people suffering from bulimia have decreased volumes of brain matter, and that the abnormalities are reversible after long-term recovery.
[43][44] Abnormal blood levels of peptides important for the regulation of appetite and energy balance are observed in individuals with bulimia nervosa, but it remains unknown if this is a state or trait.
[49] A survey of 15- to 18-year-old high school girls in Nadroga, Fiji, found the self-reported incidence of purging rose from 0% in 1995 (a few weeks after the introduction of television in the province) to 11.3% in 1998.
[51] When attempting to decipher the origin of bulimia nervosa in a cognitive context, Christopher Fairburn et al.'s cognitive-behavioral model is often considered the golden standard.
Fairburn et al. argue that extreme concern with weight and shape coupled with low self-esteem will result in strict, rigid, and inflexible dietary rules.
Accordingly, this would lead to unrealistically restricted eating, which may consequently induce an eventual "slip" where the individual commits a minor infraction of the strict and inflexible dietary rules.
[53] In contrast, Byrne and Mclean's findings differed slightly from Fairburn et al.'s cognitive-behavioral model of bulimia nervosa in that the drive for thinness was the major cause of purging as a way of controlling weight.
Consequently, body dissatisfaction coupled with a drive for thinness is thought to promote dieting and negative effects, which could eventually lead to bulimic symptoms such as purging or bingeing.
Thompson and Stice used randomized experiments (more specifically programs) dedicated to teaching young women how to be more critical when it comes to media, to reduce thin-ideal internalization.
[60] The onset of bulimia nervosa is often during adolescence, between 13 and 20 years of age, and many cases have previously experienced obesity, with many relapsing in adulthood into episodic bingeing and purging even after initially successful treatment and remission.
The diagnostic criteria includes the following:[13][64] Other methods are also used to narrow down the diagnosis, such as physical exams (measuring height, weight, and vitals, or checking skin, nails, heart and lungs), or lab tests (for blood count, electrolytes, protein, or urinalysis).
FBT involes the family in the treatment process, where parents are empowered to take an active role in helping their child recover from bulimia nervosa.
[76] Therefore, young adolescents with BN are less likely to realize the detrimental consequences of becoming bulimic and have less motivation to change,[77] which is why FBT would be useful to have families intervene and support the teens.
[74] Antidepressants, particularly selective serotonin reuptake inhibitors (SSRI), are often prescribed to treat bulimia nervosa, especially when comorbid depression or anxiety disorders are present.
[5] In addition to cognitive, genetic, and environmental factors, childhood gastrointestinal problems and early pubertal maturation also increase the likelihood of developing bulimia nervosa.
[5] Most studies conducted thus far have been on convenience samples from hospital patients, high school or university students; research on bulimia nervosa among ethnic minorities has also been limited.
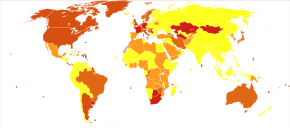
[90] According to a study conducted in 2022 by Silen et al., which conglomerated statistics using various methods such as SCID, MRFS, EDE, SSAGA, and EDDI, the US, Finland, Australia, and the Netherlands had an estimated 2.1%, 2.4%, 1.0%, and 0.8% prevalence of bulimia nervosa among females under 30 years of age.
[91] This demonstrates the prevalence of bulimia nervosa in developed, Western, first-world countries, indicating an urgency in treating adolescent women.
There are higher rates of eating disorders in groups involved in activities which idealize a slim physique, such as dance,[92] gymnastics, modeling, cheerleading, running, acting, swimming, diving, rowing and figure skating.
The first documented account of behavior resembling bulimia nervosa was recorded in Xenophon's Anabasis around 370 B.C, in which Greek soldiers purged themselves in the mountains of Asia Minor.
[106] In fact, a search for evidence of bulimia nervosa from the 17th to late 19th century revealed that only a quarter of the overeating cases they examined actually vomited after the binges.
Ellen West, a patient described by Ludwig Binswanger in 1958, was teased by friends for being fat and excessively took thyroid pills to lose weight, later using laxatives and vomiting.
[109] In 1979, Gerald Russell first published a description of bulimia nervosa, in which he studied patients with a "morbid fear of becoming fat" who overate and purged afterward.