COVID-19 drug development
[7][13][14][15] In March 2020, the WHO initiated the "SOLIDARITY Trial" in 10 countries, enrolling thousands of people infected with COVID-19 to assess treatment effects of four existing antiviral compounds with the most promise of efficacy.
[2][16] A dynamic, systematic review was established in April 2020 to track the progress of registered clinical trials for COVID-19 vaccine and therapeutic drug candidates.
[17][20][21] The term "preclinical research" is defined by laboratory studies in vitro and in vivo, indicating a beginning stage for development of a preventative vaccine, antiviral or other post-infection therapies,[7] such as experiments to determine effective doses and toxicity in animals, before a candidate compound is advanced for safety and efficacy evaluation in humans.
[22] To complete the preclinical stage of drug development – then be tested for safety and efficacy in an adequate number of people infected with COVID-19 (hundreds to thousands in different countries) – is a process likely to require 1–2 years for COVID-19 therapies, according to several reports in early 2020.
[19] Numerous candidate drugs under study as "supportive" treatments to relieve discomfort during illness, such as NSAIDs or bronchodilators, are not included in the table below.
As of May 2021, there is strong evidence that convalescent plasma treatment is not associated with clinical improvements for people with moderate or severe disease and does not decrease the risk of dying.
[69][70] This was harshly criticized by the Argentine Intensive Care Society, which stated that the trial failed to achieve its primary or secondary endpoints and did not demonstrate any statistically significant differences between the serum and placebo groups.
[80] Bebtelovimab works by binding to the spike protein of the virus that causes COVID-19, similar to other monoclonal antibodies that have been authorized for the treatment of high-risk people with mild to moderate COVID-19 and shown a benefit in reducing the risk of hospitalization or death.
[80] Bebtelovimab is a neutralizing human immunoglobulin G1 (IgG1) monoclonal antibody, isolated from a patient who has recovered from the Coronavirus disease 2019 (COVID-19), directed against the spike (S) protein of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), that can potentially be used for immunization against COVID-19.
Sotrovimab, sold under the brand name Xevudy, is a human neutralizing monoclonal antibody with activity against severe acute respiratory syndrome coronavirus 2, known as SARS-CoV-2.
[127] Molnupiravir is a prodrug of the synthetic nucleoside derivative N4-hydroxycytidine and exerts its antiviral action by introducing copying errors during viral RNA replication.
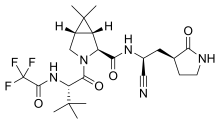
[158] Side effects of nirmatrelvir/ritonavir include changes in sense of taste (dysgeusia), diarrhea, high blood pressure (hypertension), and muscle pain (myalgia).
[19] Repurposed antiviral drugs make up most of the Chinese research, with 9 Phase III trials on remdesivir across several countries due to report by the end of April.
[19] Other potential therapeutic candidates under pivotal clinical trials concluding in March–April are vasodilators, corticosteroids, immune therapies, lipoic acid, bevacizumab, and recombinant angiotensin-converting enzyme 2, among others.
[11] In early 2020, numerous established antiviral compounds for treating other infections were being repurposed or developed in new clinical research efforts to alleviate the illness of COVID-19.
[188] The C3.ai Digital Transformation Institute, an additional consortium of Microsoft, six universities (including the Massachusetts Institute of Technology, a member of the first consortium), and the National Center for Supercomputer Applications in Illinois, working under the auspices of C3.ai, an artificial intelligence software company, are pooling supercomputer resources toward drug discovery, medical protocol development and public health strategy improvement, as well as awarding large grants to researchers who proposed by May to use AI to carry out similar tasks.
[189][190] In March 2020, the distributed computing project Folding@home launched a program to assist drug developers, initially simulating protein targets from SARS-CoV-2 and the related SARS-CoV virus, which has been studied previously.
Researchers revealed that with the help of Rosetta@home, they had been able to "accurately predict the atomic-scale structure of an important coronavirus protein weeks before it could be measured in the lab.
The partnership is a distributed computing project that "will automatically run a simulated experiment in the background [of connected home PCs] which will help predict the effectiveness of a particular chemical compound as a possible treatment for COVID-19".
[198] In March, the World Health Organization (WHO) launched the coordinated "Solidarity Trial" in 10 countries on five continents to rapidly assess in thousands of COVID-19 infected people the potential efficacy of existing antiviral and anti-inflammatory agents not yet evaluated specifically for COVID-19 illness.
[2][16] Following a study published by The Lancet on safety concerns with hydroxychloroquine, the WHO suspended use of it from the Solidarity trial in May 2020,[200][201] reinstated it after the research was retracted,[202] then abandoned further use of the drug for COVID-19 treatment when analysis showed in June that it provided no benefit.
[2] The Solidarity project is designed to give rapid insights to key clinical questions:[2][203] Enrolling people with COVID-19 infection is simplified by using data entries, including informed consent, on a WHO website.
The trial physician records and submits follow-up information about the subject status and treatment, completing data input via the WHO Solidarity website.
[29][205][207] The US National Institute of Allergy and Infectious Diseases (NIAID) initiated an adaptive design, international Phase III trial (called "ACTT") to involve up to 800 hospitalized COVID-19 people at 100 sites in multiple countries.
Beginning with use of remdesivir as the primary treatment over 29 days, the trial definition of its adaptive protocol states that "there will be interim monitoring to introduce new arms and allow early stopping for futility, efficacy, or safety.
"[38] Operation Warp Speed (OWS) was a public–private partnership initiated by the United States government to facilitate and accelerate the development, manufacturing, and distribution of COVID-19 vaccines, therapeutics, and diagnostics.
It is run by the Nuffield Departments of Public Health and of Medicine at the University of Oxford and is testing five repurposed drugs and also convalescent plasma.
[219] The trial is examining different potential therapies for severe COVID-19 infection: lopinavir/ritonavir, low-dose dexamethasone (an anti-inflammatory steroid), hydroxychloroquine, and azithromycin (a common antibiotic).
[44] On 16 June the trial group released a statement that dexamethasone had been shown to reduce mortality in patients receiving respiratory support.
Launched in December 2021, the PANORAMIC trial will test the effectiveness of molnupiravir and nirmatrelvir/ritonavir in preventing hospitalisation and helping faster recovery for people aged over 50 and those at higher risk due to underlying health conditions.