Cardiac allograft vasculopathy
Cardiac allograft vasculopathy (CAV) is a progressive type of coronary artery disease in people who have had a heart transplant.
[1] As the donor heart has lost its nerve supply there is typically no chest pain, and CAV is usually detected on routine testing.
[3] They gradually narrow and restrict its blood flow, subsequently leading to impairment of the heart muscle or sudden death.
[4] In addition to the same risk factors for coronary artery disease due to the build up of plaque, CAV is more likely to occur if the donor was older or died from explosive brain death, and if there is cytomegalovirus infection.
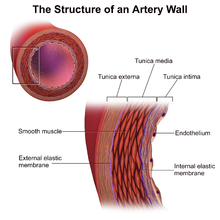
[2] Its mechanism involves immunological (innate and adaptive) and nonimmunological factors, with distinct features on histological samples of coronary arteries.
[2] Other risk factors exclusive to CAV include older donors, cytomegalovirus infection and circulating antibodies after heart transplantation.
[8] Unlike in nontransplanted people with coronary artery disease due to atherosclerosis, in CAV occlusion with thrombus of the vessel lumen is rare.
[2] Surveillance is performed by regularly repeating coronary angiography in the cardiac catheterization laboratory, the diagnostic test of choice.
[8] Biomarkers for increased risk of CAV include C-reactive protein, serum brain natriuretic peptide and troponin I have been suggested.
[8] The International Society for Heart and Lung Transplantation (ISHLT) have formulated and standardized a terminology, based on diagnostic findings, to define the presence and severity of CAV, which in turn reflects prognosis.
[2] On detection of CAV, medications including mTOR inhibitors sirolimus and everolimus have been shown to slow disease progression.
[2] Clinically significant CAV may require percutaneous coronary interventions for focal disease, but the likelihood of restenosis is high.
[12] Early survivors of heart transplants soon developed this form of vasculopathy of their coronary arteries, initially identified at post-mortems.
[12] The impact of CAV has changed over time, with early recipients being younger, having more rejection and cardiovascular risk factors and less use of statins.
[12] Future research directions in this area may include prospective databases that correlate clinical factors with surveillance of the incidence and severity of AMR, the frequency of CMV infection, and the use of immunosuppressants.