Heart failure
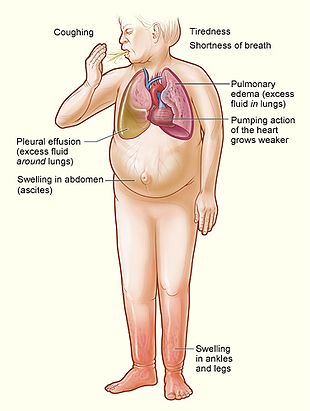
Although symptoms vary based on which side of the heart is affected, HF typically presents with shortness of breath, excessive fatigue, and bilateral leg swelling.
[26] When the heart functions poorly as a pump and does not circulate blood adequately via the circulatory system to meet the demands of the body, the term 'cardiovascular insufficiency' is sometimes used.
[30] The left side of the heart takes oxygen-rich blood from the lungs and pumps it to the rest of the circulatory system in the body (except for the pulmonary circulation).
Impaired left ventricular forward function can lead to symptoms of poor systemic perfusion such as dizziness, confusion, and cool extremities at rest.
This includes NSAIDs, COX-2 inhibitors, a number of anesthetic agents such as ketamine, thiazolidinediones, some cancer medications, several antiarrhythmic medications, pregabalin, alpha-2 adrenergic receptor agonists, minoxidil, itraconazole, cilostazol, anagrelide, stimulants (e.g., methylphenidate), tricyclic antidepressants, lithium, antipsychotics, dopamine agonists, TNF inhibitors, calcium channel blockers (especially verapamil and diltiazem[52][53]), salbutamol, and tamsulosin.
[54] By inhibiting the formation of prostaglandins, NSAIDs may exacerbate heart failure through several mechanisms, including promotion of fluid retention, increasing blood pressure, and decreasing a person's response to diuretic medications.
[55] After analyzing data from 26 studies (836,301 patients), the recent meta-analysis found that breast cancer survivors demonstrated a higher risk heart failure within first ten years after diagnosis (hazard ratio = 1.21; 95% CI: 1.1, 1.33).
[6]: 3630 [58] HFA-PEFF considers symptoms and signs, typical clinical demographics (obesity, hypertension, diabetes, elderly, atrial fibrillation), and diagnostic laboratory tests, ECG, and echocardiography.
In left ventricular failure, evidence may exist of vascular redistribution (upper lobe blood diversion or cephalization), Kerley lines, cuffing of the areas around the bronchi, and interstitial edema.
Vasopressin levels are usually increased, along with renin, angiotensin II, and catecholamines to compensate for reduced circulating volume due to inadequate cardiac output.
Johns Hopkins states that stopping tobacco use, reducing high blood pressure, physical activity, and nutrition can drastically affect the chances of developing heart disease.
[88] The goals of treatment for people with chronic heart failure are prolonging life, preventing acute decompensation, and reducing symptoms, allowing for greater activity.
In considering therapeutic options, excluding reversible causes is of primary importance, including thyroid disease, anemia, chronic tachycardia, alcohol use disorder, hypertension, and dysfunction of one or more heart valves.
In these cases, behavioral, medical and device treatment strategies exist that can provide a significant improvement in outcomes, including the relief of symptoms, exercise tolerance, and a decrease in the likelihood of hospitalization or death.
[90] The latest evidence indicates that advance care planning (ACP) may help to increase documentation by medical staff regarding discussions with participants and improve an individual's depression.
[93][94] Behavior modification is a primary consideration in chronic heart failure management programs, with dietary guidelines regarding fluid and salt intake.
An intervention is expected to be more efficacious in encouraging physical activity than the usual care if it includes Prompts and cues to walk or exercise, like a phone call or a text message.
Additional promising strategies are Graded tasks (e.g., gradual increase in intensity and duration of exercise training), Self-monitoring, Monitoring of physical activity by others without feedback, Action planning, and Goal-setting.
[99] The inclusion of regular physical conditioning as part of a cardiac rehabilitation program can significantly improve quality of life and reduce the risk of hospital admission for worsening symptoms, but no evidence shows a reduction in mortality rates as a result of exercise.
[104] European guidelines published by ESC in 2021 recommends that ARNI should be used in those who still have symptoms while on an ACE-I or ARB, beta blocker, and a mineralocorticoid receptor antagonist.
[107] In people who are intolerant of ACE-I and ARB or who have significant kidney dysfunction, the use of combined hydralazine and a long-acting nitrate, such as isosorbide dinitrate, is an effective alternate strategy.
Its narrow therapeutic window, a high degree of toxicity, and the failure of multiple trials to show a mortality benefit have reduced its role in clinical practice.
CCM is particularly suitable for the treatment of heart failure with normal QRS complex duration (120 ms or less) and has been demonstrated to improve the symptoms, quality of life, and exercise tolerance.
While this may resolve the problems associated with heart failure, the person must generally remain on an immunosuppressive regimen to prevent rejection, which has its own significant downsides.
[152] Romans used the flowering plant Drimia maritima (sea squill), which contains cardiac glycosides, for the treatment of dropsy;[153] descriptions pertaining to heart failure are also known in the civilizations of ancient India and China.
[156][157][158] The stethoscope, invented by René Laennec in 1819, x-rays, discovered by Wilhelm Röntgen in 1895, and electrocardiography, described by Willem Einthoven in 1903, facilitated the investigation of heart failure.
[162] In the meantime, cannulae (tubes) invented by English physician Reginald Southey in 1877 was another method of removing excess fluid by directly inserting into swollen limbs.
[40][162] Over the following decades, new drug classes found their place in heart failure therapeutics, including vasodilators like hydralazine; renin-angiotensin system inhibitors; and beta-blockers.
[170] There is tentative evidence of longer life expectancy and improved left ventricular ejection fraction in persons treated with bone marrow-derived stem cells.
[169] The maintenance of heart function depends on appropriate gene expression that is regulated at multiple levels by epignetic mechanisms including DNA methylation and histone post-translational modification.