Chlamydia
[1] The infection can spread to the upper genital tract in women, causing pelvic inflammatory disease, which may result in future infertility or ectopic pregnancy.
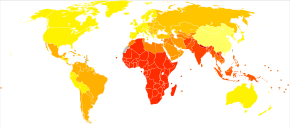
Repeated chlamydia infections of the eyes that go without treatment can result in trachoma, a common cause of blindness in the developing world.
[8] Chlamydia can be spread during vaginal, anal, oral, or manual sex and can be passed from an infected mother to her baby during childbirth.
[1][9] The eye infections may also be spread by personal contact, flies, and contaminated towels in areas with poor sanitation.
[10] Diagnosis is often by screening, which is recommended yearly in sexually active women under the age of 25, others at higher risk, and at the first prenatal visit.
[14] Chlamydia is known as the "silent epidemic", as at least 70% of genital C. trachomatis infections in women (and 50% in men) are asymptomatic at the time of diagnosis,[15] and can linger for months or years before being discovered.
If left untreated, chlamydia in men can spread to the testicles causing epididymitis, which in rare cases can lead to sterility if not treated.
Using the SAFE strategy (acronym for surgery for in-growing or in-turned lashes, antibiotics, facial cleanliness, and environmental improvements), the World Health Organization aimed (unsuccessfully) for the global elimination of trachoma by 2020 (GET 2020 initiative).
[24][25] The updated World Health Assembly neglected tropical diseases road map (2021–2030) sets 2030 as the new timeline for global elimination.
Chlamydia can affect infants by causing spontaneous abortion; premature birth; conjunctivitis, which may lead to blindness; and pneumonia.
[27] Conjunctivitis due to chlamydia typically occurs one week after birth (compared with chemical causes (within hours) or gonorrhea (2–5 days)).
[29] Chlamydia can be transmitted during vaginal, anal, oral, or manual sex or direct contact with infected tissue such as conjunctiva.
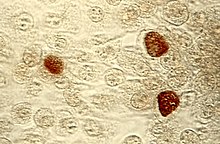
[32] The starved chlamydia bacteria can enter a persistent growth state where they stop cell division and become morphologically aberrant by increasing in size.
[33] Persistent organisms remain viable as they are capable of returning to a normal growth state once conditions in the host cell improve.
[38] In women seeking treatment in a sexually transmitted infection clinic where a urine test is negative, a subsequent cervical swab has been estimated to be positive in approximately 2% of the time.
Because of improved test accuracy, ease of specimen management, convenience in specimen management, and ease of screening sexually active men and women, the NAATs have largely replaced culture, the historic gold standard for chlamydia diagnosis, and the non-amplified probe tests.
The latter test is relatively insensitive, successfully detecting only 60–80% of infections in asymptomatic women, and often giving falsely-positive results.
Other methods also exist including: ligase chain reaction (LCR), direct fluorescent antibody resting, enzyme immunoassay, and cell culture.
[40] Rapid point-of-care tests are, as of 2020, not thought to be effective for diagnosing chlamydia in men of reproductive age and non-pregnant women because of high false-negative rates.
[42] In the United Kingdom the National Health Service (NHS) aims to: C. trachomatis infection can be effectively cured with antibiotics.
[2] Test of cure may be false-positive due to the limitations of NAAT in a bacterial (rather than a viral) context, since targeted genetic material may persist in the absence of viable organisms.