Chronic granulomatous disease
Chronic granulomatous disease (CGD), also known as Bridges–Good syndrome, chronic granulomatous disorder, and Quie syndrome,[1] is a diverse group of hereditary diseases in which certain cells of the immune system have difficulty forming the reactive oxygen compounds (most importantly the superoxide radical due to defective phagocyte NADPH oxidase) used to kill certain ingested pathogens.
[4][5] This condition was first discovered in 1950 in a series of four boys from Minnesota, and in 1957 it was named "a fatal granulomatosus of childhood" in a publication describing their disease.
[8] Bernard Babior made key contributions in linking the defect of superoxide production of white blood cells, to the cause of the disease.
Classically, patients with chronic granulomatous disease will have recurrent bouts of infection due to the decreased capacity of their immune system to fight off disease-causing organisms.
The recurrent infections they acquire are specific and are, in decreasing order of frequency:[citation needed] Most people with CGD are diagnosed in childhood, usually, before age 5.
[citation needed] Most cases of chronic granulomatous disease are transmitted as a mutation on the X chromosome and are thus called an "X-linked trait".
This has been reported in women who are homozygous for the genetic defect causing glucose-6-phosphate dehydrogenase deficiency (G6PD), which is characterised by reduced NADPH levels.
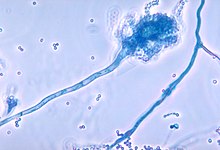
[16] Phagocytes (i.e. neutrophils and macrophages) require an enzyme to produce reactive oxygen species to destroy bacteria after they are ingested (phagocytosis), a process known as the respiratory burst.
Finally, peroxide is used by myeloperoxidase to oxidize chloride ions into hypochlorite (the active component of bleach), which is toxic to bacteria.
[3] When chronic granulomatous disease (CGD) is suspected, neutrophil-function testing should be carried out, and positive findings should be confirmed by genotyping.
[17] The p47phox mutation is due to a pseudogene conversion, hence it may not be detectable by standard sequencing; in these cases, an immunoblot or gene dose determination may be needed to confirm p47phox deficiency.
[17] DHR test is usually preferred because it is easy to use, objective, and it is able to distinguish between X-linked and autosomal forms of CGD; furthermore, it allows to detect gp91phox carriers.
As mentioned above, p47phox defect is usually difficult to identify genetically because it is caused by pseudogene conversion and may be missed in typical sequencing studies; in this case, immunoblotting or flow cytometry can show absence of protein.
[34] CGD was initially termed "fatal granulomatous disease of childhood" because patients rarely survived past their first decade in the time before routine use of prophylactic antimicrobial agents.
[8] Use of antibiotic prophylaxis, surgical abscess drainage, and vaccination led to the term "fatal" being dropped from the name of the disease as children survived into adulthood.