Cold injury
[6][7] Nonfreezing cold injuries involve tissue damage when exposed to temperatures often between 0-15 degrees Celsius for extended periods of time.
[6] While these injuries have disproportionally affected military members, recreational winter activities have also increased the risk and incidence within civilian populations.
[3] Military populations have been disproportionally affected due to prolonged cold exposure associated with work requirements.
[7] Pre-existing medical conditions that compromise blood flow, such as diabetes, Raynaud syndrome, and peripheral vascular disease increase risk of injury.
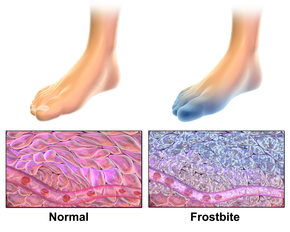
[8][11][3] Freezing causes ice crystal formation in tissue that disrupts cell membranes and surrounding blood vessels.
[11] During the rewarming process, restored blood flow induces further inflammatory damage via formation of reactive oxygen species.
[6] In suspected severe cases, magnetic resonance angiography (MRA) or Technetium-99 bone scan may be used after injury to determine the likelihood of tissue recovery and potential need for amputation.
[6][1] Bone scanning can help determine the ability to use tissue plasminogen activator (tPA) for breaking up associated blood clots.
[6] These conditions may include: Hypothermia: An accidental reduction of core body temperature to less than 35 degrees Celsius, most commonly due to cold environment exposure.
[6][10] Raynaud's phenomenon: An abnormal spasming of blood vessels often in the tips of fingers and toes - usually in response to strong emotions or cold exposure.
[10] Placing affected skin in an armpit, groin crease, or warm water bath are viable rewarming options.
[11] Choice of rewarming method depends on the suspected extent of skin injury and severity of hypothermia (if present).
[10] Surgical treatment may include removal of dead/damaged tissue (debridement) or amputation and is usually performed several weeks after initial injury.
[1] Higher degrees of injury with firm skin after rewarming, hemorrhagic blisters, and tissue necrosis or gangrene carry a worse prognosis.
[8][4] However, civilian populations with occupations that expose them to cold standing water, such as hikers,[15] or that participate in winter recreational activities are also at risk.
[4] Additional risk factors include immobility, homelessness, alcohol or tobacco abuse, elderly age, dehydration, and underlying medical conditions such as peripheral vascular disease and diabetes.
[15] This may result in destruction of small blood vessels, which leads to swelling, nerve damage, and tissue breakdown due to pressure injury.
[5] Chronic cases can occur after multiple episodes of acute injury, with partial restoration of blood flow but persistence of long-term symptoms.
[4] Other related cold-induced conditions include: Chilblains (pernio): Inflammatory skin injury that can be caused by exposure to nonfreezing cold.
[4] Rewarming should be done gradually at room temperature with affected skin exposed to air and elevated above heart level.
[5] Recommended preventative measures include minimizing skin contact with wet cold, keeping clothing warm and dry, and elevating one's feet.
[4] Chronic pain is associated with increased risk of mental health conditions, including depression, suicidal ideation, and alcohol abuse.
[6] The first mass instance of cold injury was notably documented by Baron Larrey during Napoleon's retreat from Russia in the winter of 1812-1813.
[8] Preventative measures such as rotating trench positions, changing socks multiple times per day, and using whale oil on one's feet were introduced to reduce incidence of cases.