Congenital hyperinsulinism
Congenital hyperinsulinism (HI or CHI) is a rare condition causing severe hypoglycemia (low blood sugar) in newborns due to the overproduction of insulin.
[9] Left untreated, hypoglycemia from HI can cause developmental disorders, seizures, permanent brain damage, and even death.
For those who do not respond to diazoxide, the condition is often managed with continuous carbohydrates delivered through a feeding pump and a gastrostomy tube, and off-label use of medications such as octreotide given by injection.
[5] More severe symptoms, such as seizures (fits or convulsions), can occur with a prolonged or extremely low blood sugar level.
Acquired HI may be secondary to factors around birth, such as growth restriction of the fetus, less oxygen to the baby, or maternal diabetes.
A genetic cause is also possible in children responding to diazoxide but where low sugars persist beyond the first 4 months of life.
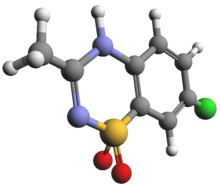
[29][30] This channel normally regulates insulin production from the β-cell in the pancreas in response to sugar levels in the blood.
In the dominant form, a single (monoallelic) change inherited from one parent (or arising spontaneously) causes diffuse HI.
Following a genetic finding, specialised positron emission tomography (PET) scanning using the radiotracer 18-fluoro-dopa can be used to localise the focal abnormality (lesion) for surgical removal.
Genetic testing is also helpful to determine if two copies of faulty ABCC8/KCNJ11 genes are inherited – these indicate a diagnosis of diffuse HI that may not respond to diazoxide.
Therefore, early rapid genetic testing is important to guide the medical and surgical management of children with severe HI.
More recently, changes in hexokinase 1 (HK1), another enzyme similar to glucokinase have been identified to cause both mild and severe forms of illness.
[39] Another sign of excess insulin action is suppressed blood levels of free fatty acids and ketones (beta-hydroxybutyrate) during hypoglycemia.
The clinical diagnosis is also supported by a large blood glucose rise after glucagon administration at the time of hypoglycemia.
[40][41][42] Glucagon is another hormone secreted from the pancreas that opposes insulin action and stimulates the release of glucose from liver glycogen stores.
[48] To prevent complications from diazoxide-induced fluid retention, diuretic therapy is typically initiated concomitantly with diazoxide.
Lack of responsiveness to diazoxide suggests the possibility that the HI is due to inactivating mutation(s) in the genes encoding the KATP channels which accounts for up to 90% of cases of diazoxide-unresponsive HI.
Off-label use of the somatostatin analogue octreotide has been the long-standing second line of treatment for HI,[50] but its effectiveness is limited by the development of tachyphylaxis.
Long-acting somatostatin analogues, octreotide LAR (administrated intramuscularly) and lanreotide (administered as a deep subcutaneous injection), are convenient options for older children.
An alternative treatment approach for diazoxide-unresponsive cases that are either not eligible or unresponsive to somatostatin analogues is the use of a continuous infusion of dextrose through a gastrostomy tube.
[12] However, up to 50% of children with the diffuse form of the disease that undergo a near-total pancreatectomy continue to have hypoglycemia after surgery requiring additional therapy.
[32] Although surgery is more likely in those with genetic forms of HI, there appears to be a reduction in severity over time, encouraging some clinicians to maintain normal glucose levels by a combination of medications such as octreotide and carbohydrate-rich feeds.
[71] More commonly, many on diazoxide develop excess body hair or a change in facial features over a long time.
By contrast, those having more extensive surgery, for example, subtotal pancreatectomy, invariably develop diabetes requiring insulin by late childhood or adolescence.
The first description of children with congenital hyperinsulinism was made in 1954 by Dr. Irvin McQuarrie in his presidential address to the American Pediatric Society.
[73] "Leucine-sensitive" hypoglycemia provided the first indication that amino acids, as well as glucose, could be important stimulators of insulin release.
[74][75][19] HI is sometimes incorrectly referred to as "nesidioblastosis", based on the appearance of the pancreatic tissue showing insulin cells arising from ductal structures.
[28] In 1964, Drash and colleagues reported that diazoxide, an antihypertensive that suppresses insulin secretion, controlled hypoglycemia in some children with HI; currently, this is the only FDA-approved drug for the treatment of hyperinsulinism.
[73] In 1996, mutations causing HI were discovered in the genes (ABCC8, KCNJ11) that encode the K-ATP channel which serves a key role in glucose-stimulated insulin secretion.
[22] Rapid genetic testing for the most common HI genes has become part of standard diagnosis and can be helpful in identifying infants likely to have a focal form of HI that can be cured by surgical removal.