Corpus luteum
While the oocyte (later the zygote if fertilization occurs) traverses the fallopian tube into the uterus, the corpus luteum remains in the ovary.
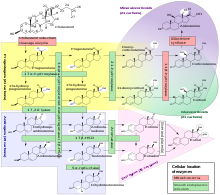
[6] The development of the corpus luteum is accompanied by an increase in the level of the steroidogenic enzyme P450scc that converts cholesterol to pregnenolone in the mitochondria.
The corpus luteum secretes progesterone, which is a steroid hormone responsible for the decidualization of the endometrium (its development) and maintenance, respectively.
[13] If the egg is not fertilised, the corpus luteum stops secreting progesterone and decays (after approximately 10 days in humans).
[14] With cessation of progesterone release, the uterine lining (functional, inner layer of the endometrium) is expelled through the vagina (in mammals that go through a menstrual cycle).
Across an estrous cycle, the functional layer regenerates to provide nourishing tissue for potential fertilisation and implantation.
[citation needed] Human chorionic gonadotropin signals the corpus luteum to continue progesterone secretion, thereby maintaining the thick lining (endometrium) of the uterus and providing an area rich in blood vessels in which the zygote(s) can develop.
[citation needed] Luteal support refers to the administration of medication (generally progestins) for the purpose of increasing the success of implantation and early embryogenesis, thereby complementing the function of the corpus luteum.
The yellow color and name of the corpus luteum, like that of the macula lutea of the retina, is due to its concentration of certain carotenoids, especially lutein.