Maternal death
[6] In higher resource regions, there are still significant areas with room for growth, particularly as they relate to racial and ethnic disparities and inequities in maternal mortality and morbidity rates.
In fact, a study published in the journal Obstetrics & Gynecology reported that in the United States, carrying a pregnancy to term and delivering a baby comes with 14 times increased risk of death as compared to a legal abortion.
Finally, a potential issue with facility-based data collection on maternal mortality is the likelihood that women who experience abortion-related complications to seek care in medical facilities.
Promoting effective contraceptive use and information distributed to a wider population, with access to high-quality care, can make steps towards reducing the number of unsafe abortions.
[27] Risk factors associated with increased maternal death include the age of the mother, obesity before becoming pregnant, other pre-existing chronic medical conditions, and cesarean delivery.
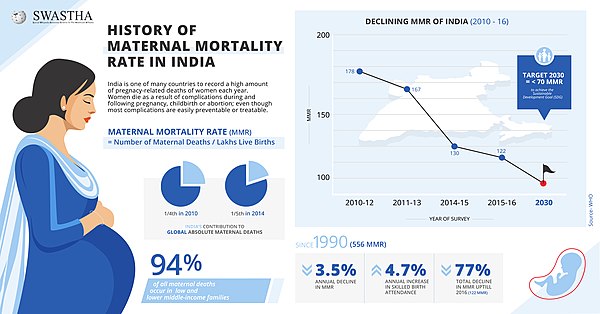
[6][43] Some factors that have been attributed to the decreased maternal deaths seen between this period are in part to the access that women have gained to family planning services and skilled birth attendance, meaning a midwife, doctor, or trained nurse), with back-up obstetric care for emergency situations that may occur during the process of labor.
[6] This can be examined further by looking at statistics in some areas of the world where inequities in access to health care services reflect an increased number of maternal deaths.
[45] In 2019, Black maternal health advocate and Parents writer Christine Michel Carter interviewed Vice President Kamala Harris.
Harris stated:"We need to speak the uncomfortable truth that women—and especially Black women—are too often not listened to or taken seriously by the health care system, and therefore they are denied the dignity that they deserve.
And we need to speak this truth because today, the United States is 1 of only 13 countries in the world where the rate of maternal mortality is worse than it was 25 years ago.
Third, emergency obstetric care to address the major causes of maternal death which are hemorrhage, sepsis, unsafe abortion, hypertensive disorders and obstructed labor.
Additionally, reliable access to information, compassionate counseling and quality services for the management of any issues that arise from abortions (whether safe or unsafe) can be beneficial in reducing the number of maternal deaths.
Studies have shown that acting on recommendations from MPDSR can reduce maternal and perinatal mortality by improving quality of care in the community and health facilities.
[52] The decline in maternal deaths has been due largely to improved aseptic techniques, better fluid management and quicker access to blood transfusions, and better prenatal care.
The non-pneumatic anti-shock garment is a low-technology pressure device that decreases blood loss, restores vital signs and helps buy time in delay of women receiving adequate emergency care during obstetric hemorrhage.
These review boards are generally comprehensive in their analysis of maternal deaths, examining details that include mental health factors, public transportation, chronic illnesses, and substance use disorders.
[58] Many states within the US are taking Maternal Mortality Review Committees a step further and are collaborating with various professional organizations to improve quality of perinatal care.
These PQCs can also involve community health organizations, Medicaid representatives, Maternal Mortality Review Committees and patient advocacy groups.
Through this collaborative effort, PQCs can aim to make impacts on quality both at the direct patient care level and through larger system devices like policy.
The PQC developed review guides and quality improvement initiatives aimed at the most preventable and prevalent maternal deaths: those due to bleeding and high blood pressure.
Access to reproductive services and sex education could make a large impact, specifically on adolescents, who are generally uneducated in regards to carrying a healthy pregnancy.
Areas for intervention have been identified in access to care, public knowledge, awareness about signs and symptoms of pregnancy complications, and improving relationships between healthcare professionals and expecting mothers.
[57] The two areas bearing the largest burden of maternal mortality, Sub-Saharan Africa and South Asia, also had the lowest percentage of births attended by a skilled provider, at just 45% and 41% respectively.
[65] Training health care professionals will be another important aspect in decreasing the rate of maternal death,[66] "The study found that white medical students and residents often believed incorrect and sometimes 'fantastical' biological fallacies about racial differences in patients.
For these assumptions, researchers blamed not individual prejudice but deeply ingrained unconscious stereotypes about people of color, as well as physicians' difficulty in empathizing with patients whose experiences differ from their own.
Researchers at the Overseas Development Institute studied maternal health systems in four apparently similar countries: Rwanda, Malawi, Niger, and Uganda.
This strategy aims to address inequalities in access to reproductive, maternal, and newborn services, as well as the quality of care with universal health coverage.
[90] There are significant maternal mortality intra-country variations, especially in nations with large equality gaps in income and education and high healthcare disparities.
It was discovered that the excess maternal death rate of women who experienced a pulmonary embolism was casually related to undergoing a cesarean delivery.
Severe Maternal Morbidity (SMM) includes any unexpected outcomes from labor or delivery that cause both short and long-term consequences to the mother's overall health.