Diabetic ketoacidosis
[1] Signs and symptoms may include vomiting, abdominal pain, deep gasping breathing, increased urination, weakness, confusion and occasionally loss of consciousness.
[6] In those with severely low blood pH who are critically ill, sodium bicarbonate may be given; however, its use is of unclear benefit and typically not recommended.
[1][6] The first full description of diabetic ketoacidosis is attributed to Julius Dreschfeld, a German-British pathologist working in Manchester, United Kingdom.
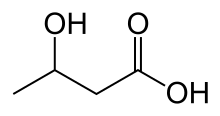
In his description, which he gave in an 1886 lecture at the Royal College of Physicians in London, he drew on reports by Adolf Kussmaul as well as describing the main ketones, acetoacetate and β-hydroxybutyrate, and their chemical determination.
[9] Various questions remain unanswered, such as whether bicarbonate administration in severe DKA makes any real difference to the clinical course, and whether an insulin loading dose is needed in adults.
Predominant symptoms are nausea and vomiting, pronounced thirst, excessive urine production and abdominal pain that may be severe.
[16] Vomiting altered blood that resembles coffee grounds occurs in a minority of people and tends to originate from erosion of the esophagus.
[6][16] On physical examination there is usually clinical evidence of dehydration, such as a dry mouth and decreased skin turgor.
[16] Small children with DKA are relatively prone to brain swelling, also called cerebral edema, which may cause headache, coma, loss of the pupillary light reflex, and can progress to death.
Young people with recurrent episodes of DKA may have an underlying eating disorder, or may be using insufficient insulin for fear that it will cause weight gain.
Furthermore, it can be triggered by severe acute illness, dehydration, extensive exercise, surgery, low-carbohydrate diets, or excessive alcohol intake.
[23] Proposed mechanisms for SGLT2-I induced "euglycemic DKA" include increased ketosis due to volume depletion combined with relative insulin deficiency and glucagon excess.
[29] High glucose levels spill over into the urine, taking water and solutes (such as sodium and potassium) along with it in a process known as osmotic diuresis.
The absence of insulin also leads to the release of free fatty acids from adipose tissue (lipolysis), which the liver converts into acetyl CoA through a process called beta oxidation.
Acetyl CoA is metabolised into ketone bodies under severe states of energy deficiency, like starvation, through a process called ketogenesis, whose final products are aceto-acetate and β-Hydroxybutyrate.
These ketone bodies can serve as an energy source in the absence of insulin-mediated glucose delivery, and is a protective mechanism in case of starvation.
Blood sugars rise, dehydration ensues, and resistance to the normal effects of insulin increases further by way of a vicious circle.
[3] The clinical state of DKA is associated, in addition to the above, with the release of various counterregulatory hormones such as glucagon and adrenaline as well as cytokines, the latter of which leads to increased markers of inflammation, even in the absence of infection.
Furthermore, markers of infection (complete blood count, C-reactive protein) and acute pancreatitis (amylase and lipase) may be measured.
[3] If cerebral edema is suspected because of confusion, recurrent vomiting or other symptoms, computed tomography may be performed to assess its severity and to exclude other causes such as stroke.
[31] Attacks of DKA can be prevented in those known to have diabetes to an extent by adherence to "sick day rules";[6] these are clear-cut instructions to patients on how to treat themselves when unwell.
Instructions include advice on how much extra insulin to take when sugar levels appear uncontrolled, an easily digestible diet rich in salt and carbohydrates, means to suppress fever and treat infection, and recommendations on when to call for medical help.
[38] The main aim in the treatment of diabetic ketoacidosis is to replace the lost fluids and electrolytes while suppressing the high blood sugars and ketone production with insulin.
Admission to an intensive care unit (ICU) or similar high-dependency area or ward for close observation may be necessary.
If dehydration is so severe as to cause shock (severely decreased blood pressure with insufficient blood supply to the body's organs), or a depressed level of consciousness, rapid infusion of saline (1 liter for adults, 10 mL/kg in repeated doses for children) is recommended to restore circulating volume.
[3][39] Slower rehydration based on calculated water and sodium shortage may be possible if the dehydration is moderate, and again saline is the recommended fluid.
[39] It is possible to use rapid acting insulin analogs injections under the skin for mild or moderate cases.
[3] Cerebral edema, if associated with coma, often necessitates admission to intensive care, artificial ventilation, and close observation.
Once this has been achieved, insulin may be switched to the usual subcutaneously administered regimen, one hour after which the intravenous administration can be discontinued.
[6][39] In people with suspected ketosis-prone type 2 diabetes, determination of antibodies against glutamic acid decarboxylase and islet cells may aid in the decision whether to continue insulin administration long-term (if antibodies are detected), or whether to withdraw insulin and attempt treatment with oral medication as in type 2 diabetes.