Fetal hemoglobin
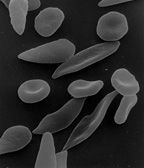
Hemoglobin F is found in fetal red blood cells, and is involved in transporting oxygen from the mother's bloodstream to organs and tissues in the fetus.
It is produced at around 6 weeks of pregnancy [1] and the levels remain high after birth until the baby is roughly 2–4 months old.
[2] Hemoglobin F has a different composition than adult forms of hemoglobin, allowing it to bind (or attach to) oxygen more strongly; this in turn enables the developing fetus to retrieve oxygen from the mother's bloodstream, which occurs through the placenta found in the mother's uterus.
Each subunit contains a heme group with an iron element which is key in allowing the binding and unbinding of oxygen.
The production of hemoglobin F starts from week 6, but it's only from 3 months onwards that it becomes the main type found in fetal red blood cells.
Thus, the key feature that allows hemoglobin F to bind more strongly to oxygen is by having γ subunits (instead of β, for example).
Alpha-thalassemia is a genetic blood disorder and one of the most common hemoglobin-related diseases, affecting the production of α subunits from hemoglobin.
[16] The disease is fatal for the fetus or newborn unless early diagnosis and intervention is carried out during pregnancy, and the child will be dependent on lifelong blood transfusions.
[18] During pregnancy, the mother's circulatory system delivers oxygen and nutrients to the fetus and carries away nutrient-depleted blood enriched with carbon dioxide.
At the same time, the decrease in carbon dioxide in fetal blood makes it more alkaline and favors the uptake of oxygen.
[20] All of these three factors are present simultaneously and cooperate to improve the fetus’ access to oxygen from the mother.
Additionally, some acquired conditions can also have higher F-cell numbers, such as acute erythropoietic stress (response to poor oxygenation which includes very rapid synthesis of new red blood cells)[23] and pregnancy.
While an early study suggested that maternal red blood cells switch on hemoglobin F production during pregnancy,[27] more recent literature suggested that the increase in haemoglobin F could be, at least in part, due to fetal red blood cells being transferred to the maternal circulation.
[28][21] Presence of high levels of hemoglobin F in pregnant women can impact the growth of the fetus, as fetal red blood cells struggle to compete for the oxygen from the mother's circulation.
[29] This is a rare benign genetic disease where production of hemoglobin F persists after twelve months of life and into the adulthood.
As a result, hemoglobin F is present in a higher number of adult red blood cells than normal.
[32] Delta beta-thalassemia is a rare genetic blood disorder in which the production of both δ and β subunits are reduced or absent.
Later, it was noted that patients with sickle cell trait as well as hereditary persistence of hemoglobin F (HPFH) didn't have symptoms.
[37] If fetal hemoglobin remains relatively high after birth, the number of painful episodes decreases in patients with sickle-cell disease and they have a better prognosis.
[39] Interestingly, while higher levels of hemoglobin F were associated with improvement of some symptoms, including the frequency of painful episodes, leg ulcers and the general severity of the disease, it had no correlation to others.
It could be that the symptoms that high hemoglobin F doesn't prevent are quite sensitive to the rupture of the sickled non-F cells.
[34] Hydroxyurea is a chemical that promotes the production of fetal hemoglobin and reduces the premature rupturing of red blood cells.
It has been suggested that elevated concentrations of haemoglobin F can be found in main kinds of solid tumours and blood cancers.