Fibromyalgia
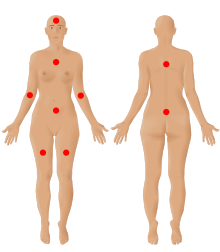
[4][13] Although a protocol using an algometer (algesiometer) for determining central sensitization has been proposed as an objective diagnostic test, fibromyalgia continues to be primarily diagnosed by exclusion despite the high possibility of misdiagnosis.
[20] Other medications commonly considered helpful in managing fibromyalgia include serotonin–norepinephrine reuptake inhibitors, nonsteroidal anti-inflammatory drugs, and muscle relaxants.
[47] The American Pain Society recognizes these problems as a major feature of fibromyalgia, characterized by trouble concentrating, forgetfulness, and disorganized or slow thinking.
[53][51] IBS and fibromyalgia share similar pathogenic mechanisms, involving immune system mast cells, inflammatory biomarkers, hormones, and neurotransmitters such as serotonin.
[73] Neuropathic pain and major depressive disorder often co-occur with fibromyalgia — the reason for this comorbidity appears to be due to shared genetic abnormalities, which leads to impairments in monoaminergic, glutamatergic, neurotrophic, opioid and proinflammatory cytokine signaling.
[87] Nociplastic pain is caused by an altered function of pain-related sensory pathways in the periphery and the central nervous system, resulting in hypersensitivity.
[19] Some suggest that fibromyalgia is caused or maintained by a decreased vagal tone, which is indicated by low levels of heart rate variability,[75] signaling a heightened sympathetic response.
[20] Glutamate/creatine ratios within the bilateral ventrolateral prefrontal cortex were found to be significantly higher in fibromyalgia patients than in controls and may disrupt glutamate neurotransmission.
Neurological effects mediated via the autonomic nervous system as well as the hypothalamic pituitary adrenal axis are directed to intestinal functional effector cells, which in turn are under the influence of the gut microbiota.
Fibromyalgia patients have less varied gut flora and altered serum metabolome levels of glutamate and serine,[110] implying abnormalities in neurotransmitter metabolism.
[111][non-primary source needed] In patients with primary fibromyalgia, studies have found disruptions in energy metabolism within skeletal muscle, including: decreased levels of ATP, ADP, and phosphocreatine, and increased levels of AMP and creatine (use of creatine kinase and myokinase in the phosphagen system due to low ATP);[112][non-primary source needed] increased pyruvate;[113][non-primary source needed] as well as reduced capillary density impairing oxygen delivery to the muscle cells for oxidative phosphorylation.
[77][non-primary source needed] Parts of the brain—the anterior cingulate cortex (ACC), thalamus, and insula—were studied using proton magnetic resonance spectroscopy (MRS) in patients with fibromyalgia and compared to healthy controls.
[77][97][non-primary source needed] There is no single pathological feature, laboratory finding, or biomarker that can diagnose fibromyalgia, and there is debate over what should be considered diagnostic criteria and whether a medical diagnosis is possible, to begin with.
[9] The new diagnosis required all of the following criteria: In 2019, the American Pain Society in collaboration with the U.S. Food and Drug Administration developed a new diagnostic system using two dimensions.
[12] Some research has suggested using a multidimensional approach taking into consideration somatic symptoms, psychological factors, psychosocial stressors and subjective belief regarding fibromyalgia.
The guidelines published by the Association of the Scientific Medical Societies in Germany[128] inform patients that self-management strategies are an important component in managing the disease.
There is strong evidence indicating that exercise improves fitness, sleep and quality of life and may reduce pain and fatigue for people with fibromyalgia.
[141] Other meta-analyses also found positive effects of tai chi for sleep,[157] fibromyalgia symptoms,[158] and pain, fatigue, depression and quality of life.
Meditative exercises, as a whole, may achieve desired outcomes through biological mechanisms such as antioxidation, anti-inflammation, reduction in sympathetic activity and modulation of glucocorticoid receptor sensitivity.
[19] Health Canada and the US Food and Drug Administration (FDA) have approved pregabalin[168] (an anticonvulsant) and duloxetine (a serotonin–norepinephrine reuptake inhibitor) for the management of fibromyalgia.
Approximately 6/10 people who take gabapentin to treat pain related to fibromyalgia experience unpleasant side effects such as dizziness, abnormal walking, or swelling from fluid accumulation.
[187] A 2016 Cochrane review concluded that there is no good evidence to support or refute the suggestion that oxycodone, alone or in combination with naloxone, reduces pain in fibromyalgia.
[189] Goldenberg et al suggest that tramadol works via its serotonin and norepinephrine reuptake inhibition, rather than via its action as a weak opioid receptor agonist.
[203][206] Two review articles found that melatonin treatment has several positive effects on fibromyalgia patients, including the improvement of sleep quality, pain, and disease impact.
[210] In a 2020 Cochrane review, cognitive behavioral therapy was found to have a small but beneficial effect for reducing pain and distress but adverse events were not well evaluated.
[232] Hyperbaric oxygen therapy (HBOT) has shown beneficial effects in treating chronic pain by reducing inflammation and oxidative stress.
Rheumatologist Frederick Wolfe, lead author of the 1990 paper that first defined the diagnostic guidelines for fibromyalgia, stated in 2008 that he believed it "clearly" not to be a disease but instead a physical response to depression and stress.
[243] Some members of the medical community do not consider fibromyalgia a disease because of a lack of abnormalities on physical examination and the absence of objective diagnostic tests.
[245] As of 2022, neurologists and pain specialists tend to view fibromyalgia as a pathology due to dysfunction of muscles and connective tissue as well as functional abnormalities in the central nervous system.
Rheumatologists define the syndrome in the context of "central sensitization" – heightened brain response to normal stimuli in the absence of disorders of the muscles, joints, or connective tissues.