Gender-affirming hormone therapy
This form of hormone therapy is given as one of two types, based on whether the goal of treatment is masculinization or feminization: Eligibility for GAHT may require an assessment for gender dysphoria or persistent gender incongruence; or many medical institutions now use an informed consent model, which ensures patients are informed of the procedure process, including possible benefits and risks, while removing many of the historical barriers needed to start hormone therapy.
The formal requirements to begin gender-affirming hormone therapy vary widely depending on geographic location and specific institution.
Gender-affirming hormones can be prescribed by a wide range of medical providers including, but not limited to, primary care physicians, endocrinologists, and gynecologists.
[2] Many international guidelines and institutions require persistent, well-documented gender dysphoria as a pre-requisite to starting gender-affirmation therapy.
[7] Signs of gender dysphoria can include comorbid mental health stressors such as depression, anxiety, low self-esteem, and social isolation.
[9] For transgender youth, the Dutch protocol existed as among the earlier guidelines for hormone therapy by delaying puberty until age 16.
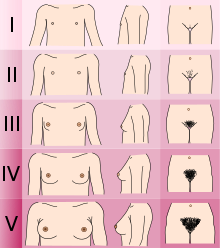
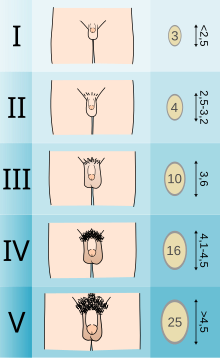
The Standards of Care set forth by WPATH recommend individuals pursuing puberty-suppressing hormone therapy wait until at least experiencing Tanner Stage 2 pubertal development.
[7] Tanner Stage 2 is defined by the appearance of scant pubic hair, breast bud development, and/or slight testicular growth.
[7] This approach temporarily shuts down the Hypothalamic-Pituitary-Gonadal (HPG) Axis, which is responsible for the production of hormones (estrogen, testosterone) that cause the development of secondary sexual characteristics in puberty.
[17] Feminizing hormone therapy is typically used by transgender women, who desire the development of feminine secondary sex characteristics.
[42][43] A study presented at ENDO 2019 (the Endocrine Society's conference) shows that even after one year of treatment with testosterone, a transgender man can preserve his fertility potential.
The healthcare provider should also obtain a thorough assessment of the patient's mental health and identify potential psychosocial factors that can affect therapy.
[41] Some organizations—but fewer than in the past—require that patients spend a certain period of time living in their desired gender role before starting hormone therapy.
[47][48] Transgender and gender non-conforming activists, such as Kate Bornstein, have asserted that RLE is psychologically harmful and is a form of "gatekeeping", effectively barring individuals from transitioning for as long as possible, if not permanently.
In a patient survey conducted by the United Kingdom's National Health Service in 2008, 5% of respondents acknowledged resorting to self-medication, and 46% were dissatisfied with the amount of time it took to receive hormone therapy.
The report concluded in part: "The NHS must provide a service that is easy to access so that vulnerable patients do not feel forced to turn to DIY remedies such as buying drugs online with all the risks that entails.
Patients must be able to access professional help and advice so that they can make informed decisions about their care, whether they wish to take the NHS or private route without putting their health and indeed their lives in danger.