Transplant rejection
[5] These antigens are located on the endothelial lining of blood vessels within the transplanted organ and, once antibodies bind, will lead to the rapid activation of the complement system.
[8] Graft failure secondary to hyperacute rejection has significantly decreased in incidence as a result of improved pre-transplant screening for antibodies to donor tissues.
[18] Since not the result of direct antigen presentation, these may not necessarily be intact MHC molecules but instead other proteins that are deemed different enough from recipient may engender a response.
[2] A third semi-direct pathway has been described in which recipient APCs present fully intact donor MHCs,[17] yet its relative contribution to acute rejection is not as well understood.
[4][6] The greater the difference in MHC between donor and recipient, the more cytotoxic T-cells are recruited to damage the graft,[6] which may be seen via biopsy in solid organ transplants, with increased lymphocyte infiltration indicative of more severe acute cellular rejection.
[4] The antibodies deposit themselves within the donor graft and lead to activation of the complement cascade alongside antibody-mediated cytotoxicity with neutrophils, a type of white blood cell separate from lymphocytes, predominantly infiltrating into tissues.
[22] While it is unknown the exact contribution of the immune system in these processes, the indirect pathway of allorecognition and the associated antibody formation seems to be especially involved.
[20] Therefore, chronic rejection explains long-term morbidity in most lung-transplant recipients,[23][24] the median survival roughly 4.7 years, about half the span versus other major organ transplants.
[25] Airflow obstruction not ascribable to other cause is labeled bronchiolitis obliterans syndrome (BOS), confirmed by a persistent drop—three or more weeks—in forced expiratory volume (FEV1) by at least 20%.
[26] First noted is infiltration by lymphocytes, followed by epithelial cell injury, then inflammatory lesions and recruitment of fibroblasts and myofibroblasts, which proliferate and secrete proteins forming scar tissue.
[29] A pilot study conducted by Michael O. Killian PhD from Florida State University and Dr. Dipankar Gupta from University of Florida published in April 2022 in Pediatric Transplantation [30] studied the acceptability and feasibility of an asynchronous directly observed therapy mobile health application among adolescent heart transplant recipients.
[citation needed] Diagnosis of acute rejection relies on clinical data—patient signs and symptoms but also calls on laboratory data such as blood or even tissue biopsy.
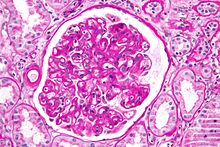
The laboratory pathologist generally seeks three main histological signs: (1) infiltrating T cells, perhaps accompanied by infiltrating eosinophils, plasma cells, and neutrophils, particularly in telltale ratios, (2) structural compromise of tissue anatomy, varying by tissue type transplanted, and (3) injury to blood vessels.
[31][32][33] Cellular magnetic resonance imaging (MRI) of immune cells radiolabeled in vivo might—similarly to Gene Expression Profiling (GEP)—offer noninvasive testing.
There is a risk of graft-versus-host disease (GVHD), however, whereby mature lymphocytes entering with marrow recognize the new host tissues as foreign and destroy them.