Heparin-induced thrombocytopenia
If someone receiving heparin develops new or worsening thrombosis, or if the platelet count falls, HIT can be confirmed with specific blood tests.
Examples of arterial thrombosis are stroke, myocardial infarction ("heart attack"), and acute leg ischemia.
These include fever, chills, high blood pressure, a fast heart rate, shortness of breath, and chest pain.
In HIT, the immune system forms antibodies against heparin when it is bound to a protein called platelet factor 4 (PF4).
However, those who have been exposed to heparin in the last few months may still have circulating IgG, as IgG-type antibodies generally continue to be produced even when their precipitant has been removed.
The timing, severity of the thrombocytopenia, the occurrence of new thrombosis, and the presence of alternative explanations, all determine the likelihood that HIT is present.
[7][11] Given the fact that HIT predisposes strongly to new episodes of thrombosis, simply discontinuing the heparin administration is insufficient.
Generally, an alternative anticoagulant is needed to suppress the thrombotic tendency while the generation of antibodies stops and the platelet count recovers.
If the patient was receiving warfarin at the time when HIT is diagnosed, the activity of warfarin is reversed with vitamin K.[1][9] Transfusing platelets is discouraged, as a theoretical risk indicates that this may worsen the risk of thrombosis; the platelet count is rarely low enough to be the principal cause of significant hemorrhage.
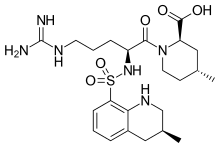
[9] Various nonheparin agents are used as alternatives to heparin therapy to provide anticoagulation in those with strongly suspected or proven HIT: danaparoid, fondaparinux, bivalirudin, and argatroban.
[citation needed] According to a systematic review, people with HIT treated with lepirudin showed a relative risk reduction of clinical outcome (death, amputation, etc.)
In addition, people treated with argatroban for HIT showed a relative risk reduction of the above clinical outcomes to be 0.20 and 0.18.
[4][16] The fact that this phenomenon occurred together with thrombocytopenia was reported in 1969;[17] prior to this time, platelet counts were not routinely performed.
[4] In 1984–1986, John G. Kelton and colleagues at McMaster University Medical School developed the laboratory tests that could be used to confirm or exclude heparin-induced thrombocytopenia.
[4][19] Treatment was initially limited to aspirin and warfarin, but the 1990s saw the introduction of a number of agents that could provide anticoagulation without a risk of recurrent HIT.
[4] In 2021 a condition resembling HIT but without heparin exposure was described to explain unusual post-vaccination embolic and thrombotic events after the Oxford–AstraZeneca COVID-19 vaccine.