Healthcare in South Korea
[5][6][7] After the Korean War ended in 1953, South Korea's medical infrastructure and healthcare system needed attention.
Due to the success it received, the Minnesota Project is accredited with pushing Korea's healthcare industry into what it is today.
Due to the current health care laws in South Korea, all of its citizens have the right to receive healthcare treatment.
This was primarily seen as a temporary adjustment to assist the South Korean Government until such a time as healthcare spending could be brought to reasonable levels and the NHI's deficit could be more easily managed.
[16] Despite being able to achieve universal health care, this program resulted in more equity issues within society as it grouped people into different categories based on demographic factors like geographical location and employment type.
[4] A major healthcare financing reform in 2000 merged all medical societies into the National Health Insurance Service (NHIS).
The four-year delay occurred because of disagreements in the legislature on how to properly assess self-employed individuals in order to determine their contribution.
[19] In 2024, the Ministry of Health and Welfare announced a 2024-28 comprehensive plan supported by more than 10 trillion won (USD 7.47 billion), with the aim to better compensate “essential but undervalued medical services to tackle the shortage of medical professionals in certain sectors, as well as target the issues of overtreatment and overspending in the national health care system.”[20] To address the high frequency of visits per year and incentivize responsible use of the national health insurance system, the ministry announced plans to adjust patient rates based on system use: patients with a demonstrated tendency to overuse will receive adjusted rates—that is, patients will be responsible for a higher percentage of the cost of treatment.
[20] In 2024, the Supreme Court of South Korea ruled in favor of a gay couple seeking spousal coverage for National Health Insurance benefits, in a landmark decision that acknowledged same-sex couples as eligible dependents to be covered, and that failure to offer coverage was an unjust discrimination without reasonable cause, thereby violating the constitutional principle of equality under Article 11 of the Constitution of the Republic of Korea that all citizens shall be equal before the law and that there shall be no discrimination in political, economic, social, or cultural life based on sex, religion, or social status.
Additionally, there was a rapid increase in the availability of advanced medical devices, including a notable growth in the number of CT and MRI machines, which are considered state-of-the-art equipment.
As a result, there is a significant concentration of patients seeking care at these renowned hospitals, creating a noticeable imbalance in healthcare utilization.
The South Korean government has failed to adequately address health disparities between urban and rural areas.
This is due to a number of factors, including the lack of access to private medical facilities in rural areas.
The South Korean government has failed to provide adequate working conditions to physicians to address health disparities.
This has led to a sense among physicians themselves that they have become mere instruments serving the interests of the government or insurance groups rather than focusing on the well-being of their patients.
Virtually, medical fees have been controlled strictly by the government and remain at a fraction of the prices in the United States, and cheaper than those in China and Singapore.
[32][33] South Korea has an insurance system with low reimbursement rates which encourages high turnover by hospitals and does little to dissuade patients from seeking second opinions.
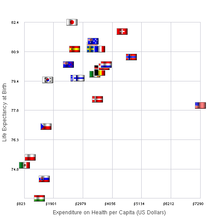
South Korea is recognized as a nation that offers excellent medical services despite the relatively low burden of public health insurance premiums.
Nonetheless, patients bear the responsibility of paying for medical services that are not covered by health insurance, which places a financial strain on them.
Healthcare providers encounter challenges due to the significantly low prices set by the health insurance system for the medical services they offer.
Healthcare providers face challenges in terms of satisfaction and burnout as they struggle to obtain sufficient treatment time due to inadequate reimbursement.
[39][40][41] In South Korea, the Health Insurance Review and Assessment Service (HIRA) lacks an objective standard for determining appropriate medical fees.
The reimbursement coverage and pricing rules for medical devices in South Korea have undergone gradual changes, including the introduction of the 'Value Appraisal Standard (VAS)' system in March 2006.
However, the VAS system has faced criticism for its lack of objectivity, transparency, and inadequate recognition of the value of innovative medical devices.
This omission ultimately resulted in governance failure, sparking unnecessary severe conflicts among key actors such as doctors, pharmacists, civil society organizations, and the news media.
These frames depict doctors as "a group primarily motivated by economic interests, violating the ethical code of their profession, suffering from internal divisions, and refusing to engage in dialogue."
Decades of declining birth rates have discouraged South Korean doctors from entering what they fear to be a field without a future.
Additionally, significant legal pressures have discouraged promising medical students from pursuing careers in obstetrics and gynecology, contributing to an aging and imbalanced gender distribution within these professions.
Simultaneously, they are expected to pursue profitability by delivering high-quality care through competition and operating as an independent, self-sustaining entity following private business principles.
The decline in inpatient revenue at local public hospitals can be attributed to several factors, including low reimbursement rates, the provision of charitable care to individuals with low incomes, and the delivery of low-revenue-generating services such as obstetrics and gynecology and pediatric services in medically underserved regions.