Hiatal hernia
[1] Symptoms from a hiatal hernia may be improved by changes such as raising the head of the bed, weight loss, and adjusting eating habits.
Among them, a person with a hiatal hernia can experience dull pains in the chest, shortness of breath (caused by the hernia's effect on the diaphragm), heart palpitations (due to irritation of the vagus nerve), and swallowed food "balling up" and causing discomfort in the lower esophagus until it passes on to the stomach.
In newborns, the presence of Bochdalek hernia can be recognised[4] from symptoms such as difficulty breathing,[5] fast respiration, and increased heart rate.
The diagnosis of a hiatal hernia is typically made through an upper GI series, endoscopy, high resolution manometry, esophageal pH monitoring, and computed tomography (CT).
Barium swallow as in upper GI series allows the size, location, stricture, stenosis of oesophagus to be seen.
CT scan is useful in diagnosing complications of hiatal hernia such as gastric volvulus, perforation, pneumoperitoneum, and pneumomediastinum.
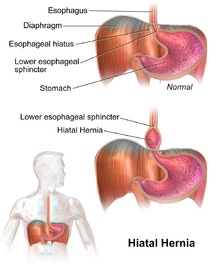
[11] There is a widening of the muscular hiatal tunnel and circumferential laxity of the phrenoesophageal ligament, allowing a portion of the gastric cardia to herniate upward into the posterior mediastinum.
Although type II hernias are associated with reflux disease, their primary clinical significance lies in the potential for mechanical complications.
[citation needed] There is tentative evidence from non-controlled trials that oral neuromuscular training may improve symptoms.
With proper patient selection, laparoscopic fundoplication studies in the 21st century have indicated relatively low complication rates, quick recovery, and relatively good long term results.
[17][18][19][20] Regarding the discussion of partial versus complete fundoplication procedures, significant variations in the postoperative outcome emphasize the increased prevalence of dysphagia after Nissen.
The statistics given support the superiority of laparoscopic over traditional surgery, owing to the greater aesthetic result, shorter admission time – with lower costs – and faster social reintegration.
[citation needed] Hiatal hernias are most common in North America and Western Europe and rare in rural African communities.
Other risk factors for the condition include: nasal masses, laryngeal paralysis, and a narrowed intrapharyngeal opening.
[25] Treatment of airway obstructions and feeding low-fat more digestible food can alleviate any need for invasive procedures.