History and naming of human leukocyte antigens
The antigens were initially identified by categorizing and performing massive statistical analyses on interactions between blood types.
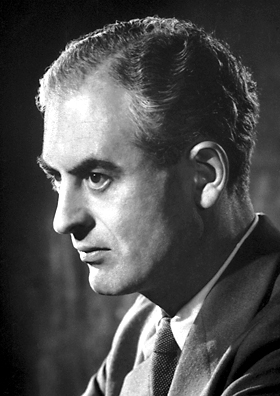
The thought that the mammalian body must have some way of identifying introduced foreign tissues first arose during World War II.
A plane crash near his home changed the path of his career, turning his work with burns from mere academia to a full on quest to save lives.
Medawar and a Scottish surgeon, Tom Gibson, were tasked with working the Burns Unit of the Glasgow Royal Infirmary.
Successive skin grafts from the brother were destroyed even faster, a fact that gave them the evidence they needed to implicate the immune system.
[1] Burnet, independently of Medawar, came to the conclusion that the immune system must learn to tolerate any self cells, and hypothesized that this must occur during fetal development.
Burnet's work continued and in 1957 along with Niels Jerne published a paper that modified and revolutionized antibody theory.
At the time, many leading scientists including Linus Pauling and James Watson completely rejected the idea, but repeated experimentation intended to disprove the theory actually served to build up a large body of evidence supporting Burnet and Jerne's theory.
[1] The biggest weakness in Burnet's theory was that he had no explanation for how the body selected for immune cells that only identified non-self.
[1] In 1958 Jean Dausset, Jon van Rood and Rose Payne published papers in which they described antibodies in human sera that reacted with the leucocytes from many but not all other tested individuals.
Thus he detected an alloantigen on human leucocytes which he subsequently named MAC after the initials of three important volunteers for his experiments.
[7] At this point the researchers all realized that the sheer quantity of data they were capable of obtaining was vastly greater than that of any previous study and so collaboration would be essential.
Different experimental methods and inconsistency in the execution of the same tests and a non-homogeneity of naming systems added together to make collaboration incredibly difficult.
This in turn would aid in organization and would more easily facilitate the unification of data being collected at numerous laboratories across the world.
Late in 1973 a pair of researchers in Australia, Rolf Zinkernagel and Peter Doherty made a revelatory discovery that altered the thinking of immunologists forever.
After looking at the MHCs present in the mice, they realized that cytotoxic T-cells could only identify virus infections in cells with the right Class I compatibility gene.
Traditional thinking was that the immune system identified infections directly but this discovery turned that theory on its head.
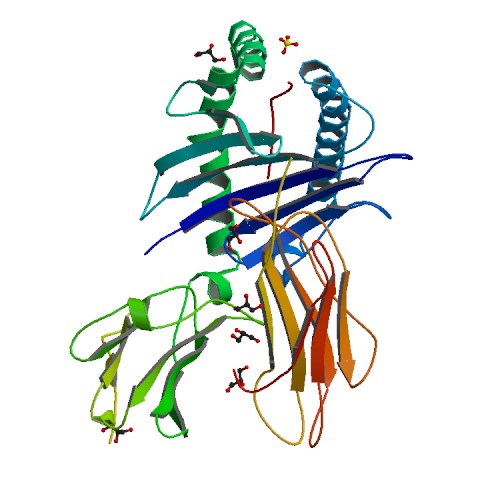
[11] It took a team of three researchers at Harvard, Don Wiley, Jack Strominger, and Pamela Bjorkman, eight years to ferret out the structure of the HLA protein.
They completed their work in the spring of 1987, discovering that the final 10% made a "cup" (of sorts) located on top of the molecule.
The third set of numbers (HLA-A*02:101:01) indicates an allele variant that has a different DNA sequence but produces the same protein as the normal gene.
The final set of numbers (HLA-A*02:101:01:01) is used to designate a single or multiple nucleotide polymorphism in a non-coding region of the gene.
The "A4" subset evolved to become D-region antigens, which was a large cluster of genes that encoded MHC class II.
The D-region has 8 major coding loci that combine to form 3 different protein groups; DP, DQ, and DR. DRw antigens were the first to be split, a process made easy by the virtue of having an invariant alpha chain, but complicated by 4 beta chain loci (DRB1, DRB3, DRB4, and DRB5).
To explain rejection in a nutshell, certain immune system components are highly variable, the agents are called the Major histocompatibility (MHC) antigens.
Patients received skin, white blood cell or kidney donations from other donors (called allografts, meaning 'of different genetics' grafts).
If these allografts were rejected, it was found that the 'rejection' response was accompanied by an antibody mediated agglutination of red blood cells (See figure).
It would have taken substantially longer to identify other alleles because frequencies were lower, and haplotypes that migrated into the European population had undergone equilibration or were from multiple sources.
In the late 1960s, scientist began reacting sera from patients with rejecting transplants to donor or 'third party' tissues.
The first major observation, in 1969, was that an allotypic antibodies to "4" ("Four") was only found on lymphocytes, while most of the antigens, termed "LA", recognized most cells in the body.
A series of tests on cultured cells revealed that, within the "LA" group, a donor tissue might have some antigens but not others.


A1, A2, B7, B8 do not cause reaction because they are in both donor and recipient, DR2 and DR3 are found on lymphoid cells
