Hyphema
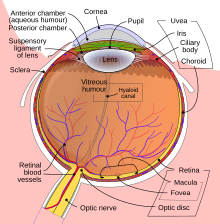
[1] The person's vision may improve over time as the blood moves by gravity lower in the anterior chamber of the eye, between the iris and the cornea.
[1] Traumatic hyphema may lead to increased intraocular pressure (IOP), peripheral anterior synechiae, atrophy of the optic nerve, staining of the cornea with blood, re-bleeding, and impaired accommodation.
[3] Secondary hemorrhage, or rebleeding of the hyphema, is thought to worsen outcomes in terms of visual function and lead to complications such as glaucoma, corneal staining, optic atrophy, or vision loss.
Spontaneous hyphemas are usually caused by the abnormal growth of blood vessels (neovascularization), tumors of the eye (retinoblastoma or iris melanoma), uveitis, or vascular anomalies (juvenile xanthogranuloma).
[2] Additional causes of spontaneous hyphema include: rubeosis iridis, myotonic dystrophy, leukemia, hemophilia, and von Willebrand disease.
[citation needed] The main goals of treatment are to decrease the risk of re-bleeding within the eye, corneal blood staining, and atrophy of the optic nerve.
Aspirin and ibuprofen should be avoided, because they interfere with platelets' ability to form a clot and consequently increase the risk of additional bleeding.
Aminocaproic or tranexamic acids are often prescribed for hyphema on the basis that they reduce the risk of rebleeding by inhibiting the conversion of plasminogen to plasmin, and thereby keeping clots stable.