Hypothyroidism
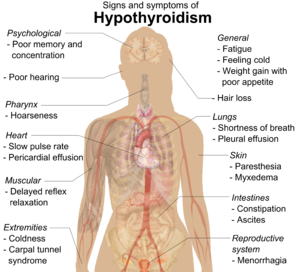
[3] It can cause a number of symptoms, such as poor ability to tolerate cold, extreme fatigue, muscle aches, constipation, slow heart rate, depression, and weight gain.
[3] Untreated cases of hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby or congenital iodine deficiency syndrome.
Numerous symptoms and signs are associated with hypothyroidism and can be related to the underlying cause, or a direct effect of not having enough thyroid hormones.
[17] Delayed relaxation after testing the ankle jerk reflex is a characteristic sign of hypothyroidism and is associated with the severity of the hormone deficit.
People with myxedema coma typically have a low body temperature without shivering, confusion, a slow heart rate and reduced breathing effort.
[22][27][28][29] Newborn children with hypothyroidism may have normal birth weight and height (although the head may be larger than expected and the posterior fontanelle may be open).
[31] Normal growth and development may be delayed, and not treating infants may lead to an intellectual impairment (IQ 6–15 points lower in severe cases).
Other problems include the following: difficulty with large scale and fine motor skills and coordination, reduced muscle tone, squinting, decreased attention span, and delayed speaking.
[32] In older children and adolescents, the symptoms of hypothyroidism may include fatigue, cold intolerance, sleepiness, muscle weakness, constipation, a delay in growth, overweight for height, pallor, coarse and thick skin, increased body hair, irregular menstrual cycles in girls, and delayed puberty.
[8] Iatrogenic hypothyroidism can be surgical (a result of thyroidectomy, usually for thyroid nodules or cancer) or following radioiodine ablation (usually for Graves' disease).
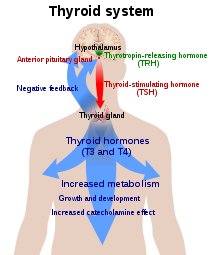
In healthy individuals, the thyroid gland predominantly secretes thyroxine (T4), which is converted into triiodothyronine (T3) in other organs by the selenium-dependent enzyme iodothyronine deiodinase.
[41] Triiodothyronine binds to the thyroid hormone receptor in the nucleus of cells, where it stimulates the turning on of particular genes and the production of specific proteins.
Production of TSH by the anterior pituitary gland is stimulated in turn by thyrotropin-releasing hormone (TRH), released from the hypothalamus.
[44] Antibodies against TPO may be important in making treatment decisions, and should, therefore, be determined in women with abnormal thyroid function tests.
In addition to promoting the consumption of iodine-rich foods such as dairy and fish, many countries with moderate iodine deficiency have implemented universal salt iodization.
[57] As many women will not achieve this from dietary sources alone, the American Thyroid Association recommends a 150 μg daily supplement by mouth.
[62] Guidelines for England and Wales from the National Institute for Health and Care Excellence (NICE) recommend testing for thyroid disease in people with type 1 diabetes and new-onset atrial fibrillation, and suggests testing in those with depression or unexplained anxiety (all ages), in children with abnormal growth, or unexplained change in behavior or school performance.
[9][16][66] In 2007, the British Thyroid Association stated that combined T4 and T3 therapy carried a higher rate of side effects and no benefit over T4 alone.
A 2012 guideline from the European Thyroid Association recommends that support should be offered concerning the chronic nature of the disease and that other causes of the symptoms should be excluded.
The addition of liothyronine should be regarded as experimental, initially only for a trial period of 3 months, and in a set ratio to the current dose of levothyroxine.
[69] This extract was once a mainstream hypothyroidism treatment, but its use today is unsupported by evidence;[9][16] British Thyroid Association and American professional guidelines discourage its use,[8][67] as does NICE.
[72] A 2007 review found no benefit of thyroid hormone replacement except for "some parameters of lipid profiles and left ventricular function".
[17] Myxedema coma or severe decompensated hypothyroidism usually requires admission to the intensive care, close observation and treatment of abnormalities in breathing, temperature control, blood pressure, and sodium levels.
Mechanical ventilation may be required, as well as fluid replacement, vasopressor agents, careful rewarming, and corticosteroids (for possible adrenal insufficiency which can occur together with hypothyroidism).
Careful correction of low sodium levels may be achieved with hypertonic saline solutions or vasopressin receptor antagonists.
[19] For rapid treatment of hypothyroidism, levothyroxine or liothyronine may be administered intravenously, particularly if the level of consciousness is too low to be able to safely swallow medication.
[76] Women with anti-TPO antibodies who are trying to become pregnant (naturally or by assisted means) may require thyroid hormone supplementation even if the TSH level is normal.
[9] The severity of myxedema, and its associated risk of mortality and complications, created interest in discovering effective treatments for hypothyroidism.
[82] In 1891, the English physician George Redmayne Murray introduced subcutaneously injected sheep thyroid extract,[83] followed shortly after by an oral formulation.
After hypothyroidism was found to cause a lower basal metabolic rate, this was used as a marker to guide adjustments in therapy in the early 20th century (around 1915).