Imaging informatics
These include DICOM (Digital Imaging and Communications in Medicine), Health Level 7 (HL7), International Organization for Standardization (ISO), and Artificial Intelligence protocols.
As a result, the main limiting factor for the medical imaging field became the human inability to accurately interpret large amounts of data.
The world quickly realized that digital imaging standards would need to be put in place given the impact PACS had on the medical community.
The American College of Radiology (ACR) and the National Electrical Manufacturers Association (NEMA) created the Digital Imaging and Communications Standards Committee (later becoming DICOM) in response to this concern.
[4] Although a highly accurate and fully automated CAD system has yet to be realized, recent advancements in Artificial Intelligence may allow for functioning implementations.
The expeditious advancement in this field necessitates a vigilant approach to sustain uniformity, foster interoperability, and guarantee the efficacious dissemination of imaging data.
[12] DDInteract has been crafted to enhance cooperative engagement between healthcare practitioners and patients, aiming to ascertain the optimal therapeutic approach that minimizes the hazards posed by potential drug-drug interactions.
[13] A systematic review critically assessed the design, reporting standards, risk of bias, and validity of claims within studies that compare the efficacy of diagnostic deep learning algorithms in medical imaging against the expertise of clinicians.
Conducted using data from prominent databases spanning from 2010 to June 2019, the review specifically targeted studies involving convolutional neural networks (CNNs)—notable for their capacity to autonomously discern crucial features for image classification within medical contexts.
The investigation uncovered a notable deficiency in randomized clinical trials concerning this subject, identifying only ten such studies, of which merely two were published, exhibiting low risk of bias and commendable adherence to reporting protocols.
Among the 81 non-randomized studies located, a minority were prospective or validated in practical clinical settings, with the majority presenting a high risk of bias, substandard compliance with reporting norms, and a pronounced lack of accessibility to data and code.
This review underscores the imperative for an augmentation in the number of prospective studies and randomized trials, advocating for diminished bias, amplified clinical pertinence, enhanced transparency, and tempered conclusions in the burgeoning field of applying deep learning to medical imaging.
[14] The exponential growth in digital data alongside enhanced computing capabilities has markedly accelerated advancements in artificial intelligence (AI), which are now progressively being incorporated into healthcare.
In response, we propose MINIMAR (Minimum Information for Medical AI Reporting), an initiative designed to establish critical parameters for understanding AI-driven predictions, the demographics targeted, inherent biases, and the ability to generalize these technologies.
We urge the adoption of standardized protocols to ensure that AI implementations in healthcare are reported with accuracy and responsibility, facilitating the development and deployment of associated clinical decision-support tools while simultaneously addressing critical concerns regarding precision and bias.
Through various clinical decision support systems(CDSS), professionals can ease the manual labor of tissue region selection, using Whole-Slide Imaging(WSI) tools to maximize the information analyzed.
[22] The expansion of DICOM standards facilitated the widespread adoption of Picture Archiving and Communication Systems (PACS), marking a milestone in the digital transformation of imaging informatics.
[23] The field of radiomics, which involves extracting quantitative features from medical images that are invisible to the human eye, saw significant growth towards the late 2010s.
These detectors offer a more efficient process for converting X-rays to electrical signals, allowing for better material differentiation and potentially reducing the radiation dose for patients.
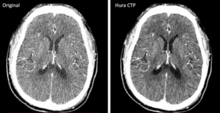
Deep learning, a subset of ML, is particularly pivotal in transforming radiological imaging, with algorithms increasingly being developed for tasks such as tumor detection, organ segmentation, and anomaly identification.
[11][25] Looking ahead, the future directions of imaging informatics are expected to further embrace interdisciplinary approaches, incorporating genetics, pathology, and data from wearable devices to offer more holistic views of patient health.
The concept of "radiogenomics," linking imaging features with genomic data, is an area of growing interest, potentially leading to more personalized and precise medical treatments.
Advances in technology must be balanced with considerations of practicality, ethics, and equity to ensure that imaging informatics can fulfill its promise to enhance patient care and treatment outcomes.
For example, the development of handheld ultrasound devices has revolutionized point-of-care imaging by providing clinicians with portable and easy-to-use tools for bedside examinations (Smith, 2018).
For instance, recent studies have demonstrated the effectiveness of combining MRI, CT, and ultrasound data for improved diagnosis and treatment planning in oncology patients (Gupta et al., 2020).
[29] By fusing data from these sources, clinicians can obtain a more comprehensive understanding of a patient's condition, leading to more accurate diagnoses and personalized treatment plans.