Inflammatory bowel disease
[9][10] Associated complaints or diseases include arthritis, pyoderma gangrenosum, primary sclerosing cholangitis, and non-thyroidal illness syndrome (NTIS).
[14] IBD is a complex disease which arises as a result of the interaction of environmental and genetic factors leading to immunological responses and inflammation in the intestine.
[22][23] A 2022 study found that diets with increased intake of fruits and vegetables, reduction of processed meats and refined carbohydrates, and preference of water for hydration were associated with lower risk of active symptoms with IBD, although increased intake of fruits and vegetables alone did not reduce risk of symptoms with Crohn's disease.
[24] A 2022 scientific review also found generally positive outcomes for IBD patients who adhered to the Mediterranean diet (high fruit and vegetable intake).
[35] Another opportunistic bacterium called A. muciniphila contributes to IBD development and is more prevalent in individuals lacking NOD-like receptor 6 (NLRP6).
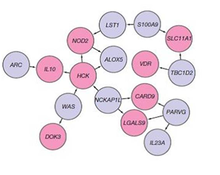
Other studies show that mutations in IBD-associated genes might interfere with the cellular activity and interactions with the microbiome that promote normal immune responses.
[52] By 2020, single-cell RNA sequencing analysis was launched by a small consortium using IBD patient biopsy material in a search for therapeutic targets.
Crohn's can affect any part of the gastrointestinal tract, from mouth to anus (skip lesions), although a majority of the cases start in the terminal ileum.
[64] Microscopically, ulcerative colitis is restricted to the mucosa (epithelial lining of the gut), while Crohn's disease affects the full thickness of the bowel wall ("transmural lesions").
[66] Irritable bowel syndrome can present with similar symptoms as either disease, as can nonsteroidal anti-inflammatory drug (NSAID) enteritis and intestinal tuberculosis.
[84] Low serum levels of alanine transaminase can be a marker of sarcopenia which is underdiagnosed in patients with IBD and associated with a higher disease activity.
[90] There is some evidence that vitamin D supplementation therapy may be associated with improvements in scores for clinical inflammatory bowel disease activity and biochemical markers.
[92][93] The use of oral probiotic supplements to modify the composition and behaviour of the microbiome has been considered as a possible therapy for both induction and maintenance of remission in people with Crohn's disease and ulcerative colitis.
Systematic reviews showed that 33% of ulcerative colitis, and 50% of Crohn's disease patients reach clinical remission after fecal microbiota transplant.
A review of studies suggests a promising role, although there are substantial challenges, including cost and characterization of effects, which limit the current use in clinical practice.
[103][104] Currently, there is no evidence to recommend psychological treatment, such as psychotherapy, stress management and patient's education, to all adults with IBD in general.
[105] In adolescents population such treatments may be beneficial on quality of life and depression, although only short-term effects have been found, which also imposes the need for further research.
[105] A meta analysis of interventions to improve mood (including talking therapy, antidepressants, and exercise) in people with IBD found that they reduced inflammatory markers such as C-reactive protein and faecal calprotectin.
[113] Around one-third of individuals with IBD experience persistent gastrointestinal symptoms similar to irritable bowel syndrome (IBS) in the absence of objective evidence of disease activity.
[115] The cause of these IBS-like symptoms is unclear, but it has been suggested that changes in the gut-brain axis, epithelial barrier dysfunction, and the gut flora may be partially responsible.
IBD carries a psychological burden due to stigmatization of being diagnosed, leading to high levels of anxiety, depression, and a general reduction in the quality of life.
[135] In severely ill people with IBD there is a risk of the passage of viable bacteria from the gastrointestinal tract to the internal organs (bacterial translocation) and subsequent bacteremia, which can cause serious adverse health consequences.
It is believed that in a healthy gut, natural endogenous cannabinoids are released from endothelial cells when they are injured, which then bind to the CB1 receptors.
CB2, another cannabinoid receptor predominantly expressed by immune cells, was detected in the gut of people with IBD at a higher concentration.
[138] Alicaforsen is a first generation antisense oligodeoxynucleotide designed to bind specifically to the human ICAM-1 messenger RNA through Watson-Crick base pair interactions in order to subdue expression of ICAM-1.
[139] Increased expression of ICAM-1 has been observed within the inflamed intestinal mucosa of people with ulcerative colitis, pouchitis and Crohn's, where ICAM-1 over production correlated with disease activity.
[143] In 2014, an alliance among the Broad Institute, Amgen and Massachusetts General Hospital formed with the intention to "collect and analyze patient DNA samples to identify and further validate genetic targets.
[147] IBD-disease activity may impact quality of life and over time may significantly affect individual's mental well-being, which may be related to the increased risk to develop anxiety and/or depression.
[152][153] IBD also occurs in dogs and is thought to arise from a combination of host genetics, intestinal microenvironment, environmental components and the immune system.
After having excluded other diseases that can lead to vomiting, diarrhea, and abdominal pain in dogs, intestinal biopsies are often performed to investigate what kind of inflammation is occurring (lymphoplasmacytic, eosinophilic, or granulomatous).