Interferon beta-1b
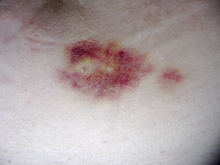
[2] Mild skin reactions usually do not impede treatment whereas necroses appear in around 5% of patients and lead to the discontinuation of the therapy.
[2] Also over time, a visible dent at the injection site due to the local destruction of fat tissue, known as lipoatrophy, may develop.
[2][4] This reaction tends to disappear after 3 months of treatment and its symptoms can be treated with over-the-counter nonsteroidal anti-inflammatory drugs, such as ibuprofen, that reduce fever and pain.
[2] Interferon-beta can also reduce numbers of white blood cells (leukopenia), lymphocytes (lymphopenia) and neutrophils (neutropenia), as well as affect liver function.
[2] Nevertheless, recommendation is that all patients should be monitored through laboratory blood analyses, including liver function tests, to ensure safe use of interferons.
Side effects are often onerous enough that many patients ultimately discontinue taking Interferons (or glatiramer acetate, a comparable disease-modifying therapies requiring regular injections).
During a CIS, there is a subacute attack suggestive of demyelination but the patient does not fulfill the criteria for diagnosis of multiple sclerosis.
[5] Treatment with interferons after an initial attack decreases the risk of developing clinical definite MS.[4][6] Medications are modestly effective at decreasing the number of attacks in relapsing-remitting multiple sclerosis[7] and in reducing the accumulation of brain lesions, which is measured using gadolinium-enhanced magnetic resonance imaging (MRI).