Jaundice
Jaundice, also known as icterus, is a yellowish or greenish pigmentation of the skin and sclera due to high bilirubin levels.
[3][6] Jaundice in adults is typically a sign indicating the presence of underlying diseases involving abnormal heme metabolism, liver dysfunction, or biliary-tract obstruction.
[10] High unconjugated bilirubin may be due to excess red blood cell breakdown, large bruises, genetic conditions such as Gilbert's syndrome, not eating for a prolonged period of time, newborn jaundice, or thyroid problems.
[4] Other conditions can also cause yellowish skin, but are not jaundice, including carotenemia, which can develop from eating large amounts of foods containing carotene—or medications such as rifampin.
[5] Jaundice in newborns may be treated with phototherapy or exchanged transfusion depending on age and prematurity when the bilirubin is greater than 4–21 mg/dl (68–365 μmol/L).
[11][12] The most common signs of jaundice in adults are a yellowish discoloration of the white area of the eye (sclera) and skin[13] with scleral icterus presence indicating a serum bilirubin of at least 3 mg/dl.
[14] Other common signs include dark urine (bilirubinuria) and pale (acholia) fatty stool (steatorrhea).
Traditionally referred to as scleral icterus, this term is actually a misnomer, because bilirubin deposition technically occurs in the conjunctival membranes overlying the avascular sclera.
Disorders associated with a rise in serum levels of conjugated bilirubin during early development can also cause dental hypoplasia.
[20] Jaundice is a sign indicating the presence of an underlying diseases involving abnormal bilirubin metabolism, liver dysfunction, or biliary-tract obstruction.
The three categories are: Prehepatic jaundice is most commonly caused by a pathological increased rate of red blood cell (erythrocyte) hemolysis.
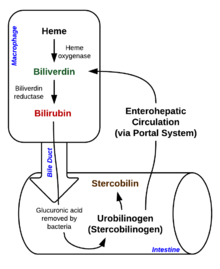
A deeper understanding of the anatomical flow of normal heme metabolism is essential to appreciate the importance of prehepatic, hepatic, and posthepatic categories.
The first oxidation reaction is catalyzed by the microsomal enzyme heme oxygenase and results in biliverdin (green color pigment), iron, and carbon monoxide.
Roughly 20% comes from other heme sources, however, including ineffective erythropoiesis, and the breakdown of other heme-containing proteins, such as muscle myoglobin and cytochromes.
In addition, subsequent cellular edema due to inflammation causes mechanical obstruction of the intrahepatic biliary tract.
[35] Most people presenting with jaundice have various predictable patterns of liver panel abnormalities, though significant variation does exist.
Other primary lab tests for liver function include gamma glutamyl transpeptidase (GGT) and prothrombin time (PT).
[37] Some bone and heart disorders can lead to an increase in ALP and the aminotransferases, so the first step in differentiating these from liver problems is to compare the levels of GGT, which are only elevated in liver-specific conditions.
[citation needed] Laboratory results for liver panels are frequently compared by the magnitude of their differences, not the pure number, as well as by their ratios.
Acute hepatitis typically has ALT and AST levels rising 20–30 times normal (above 1000) and may remain significantly elevated for several weeks.
[citation needed] Laboratory findings depend on the cause of jaundice: Unconjugated bilirubin is hydrophobic, so cannot be excreted in urine.
[39] Urobilinogen will be greater than 2 units, as hemolytic anemia causes increased heme metabolism; one exception being the case of infants, where the gut flora has not developed).
Newborns are especially vulnerable to hyperbilirubinemia-induced neurological damage, so must be carefully monitored for alterations in their serum bilirubin levels.
In the developing world, the most common cause of jaundice is infectious such as viral hepatitis, leptospirosis, schistosomiasis, or malaria.
[4] Risk factors associated with high serum bilirubin levels include male gender, white ethnicities, and active smoking.
[51] Other symptoms may include drowsiness, poor feeding, and in severe cases, unconjugated bilirubin can cross the blood-brain barrier and cause permanent neurological damage (kernicterus).
[citation needed] While most cases of newborn jaundice are not harmful, when bilirubin levels are very high, brain damage—kernicterus—may occur[55][8] leading to significant disability.
[9] A bili light is often the tool used for early treatment, which consists of exposing the baby to intensive phototherapy, which may be intermittent or continuous.
[59] A 2021 Cochrane systematic review found that sunlight can be used to supplement phototherapy, as long as care is taken to prevent overheating and skin damage.
[60] Bilirubin count is also lowered through excretion—bowel movements and urination—so frequent and effective feedings are vital measures to decrease jaundice in infants.