Lichen planus
Lichen planus (LP) is a chronic inflammatory and autoimmune disease that affects the skin, nails, hair, and mucous membranes.
[3] It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale (Wickham's striae), commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa.
[5] Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement.
This description is known as the characteristic "6 Ps" of lichen planus: planar (flat-topped), purple, polygonal, pruritic, papules, and plaques.
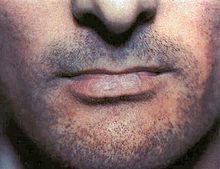
Oral lichen planus (OLP) tends to present bilaterally as mostly white lesions on the inner cheek,[41] although any mucosal site in the mouth may be involved.
Other sites, in decreasing order of frequency, may include the tongue, lips, gingivae, floor of the mouth, and very rarely, the palate.
[41] Generally, oral lichen planus tends not to cause any discomfort or pain, although some people may experience soreness when eating or drinking acidic or spicy foodstuffs or beverages.
Additionally, the Koebner phenomenon (the development of new lesions at sites of trauma) is not only present in cutaneous lichen planus (CLP) but can also occur in the setting of OLP.
Residual postinflammatory hyperpigmentation has been reported in association with OLP, manifesting as brown to black pigmentation on the oral mucosa and may most likely occur in dark-skinned individuals.
[44] Upregulation of intercellular adhesion molecule-1 (ICAM-1) and cytokines associated with T-helper 1 immune response, may also play an important role in the pathogenesis of lichen planus.
Patients with anxiety and depression are reported more commonly with oral LP if compared to normal healthy individuals.
Other mechanisms that have been proposed include: Oral LP may also be caused by genetic factor which influence the immune function.
A separate study performed in China[52] found an association between a polymorphism in the TNF-alpha gene and risk for oral LP in a subset of patients.
An Italian study found a significant increase in a genetic polymorphism of the first intron of the interferon (IFN)-gamma promoter in patients with oral LP compared with controls.
Direct immunofluorescence (DIF) can be useful in patients with bullous lesions to differentiate the condition from an autoimmune vesiculobullous disease.
[55] A diagnosis of oral lichen planus (LP) is confirmed through review of the patient history, physical examination, and histologic findings.
[56][57] Lichenoid drug eruptions may be caused by a variety of systemic medications and share clinical features with oral LP.
Histologic findings of a deep mixed infiltrate with lymphocytes, plasma cells, and neutrophils (with or without eosinophils) and perivascular inflammation favor this diagnosis.
[59] Oral squamous cell carcinoma (SCC) can present as erythematous or white patches, ulcers, or exophytic masses.
Patients present with white plaques or erythematous patches on the buccal mucosa, palate, tongue, or oropharynx that may be mistaken for reticular LP.
Narrow band UVB phototherapy or systemic PUVA therapy are known treatment modalities for generalized disease.
[44] Reassurance that the condition is benign, elimination of precipitating factors and improving oral hygiene are considered initial management for symptomatic OLP, and these measures are reported to be useful.
[73] In contrast to cutaneous LP, which is self limited, lichen planus lesions in the mouth may persist for many years,[67] and tend to be difficult to treat, with relapses being common.
[75][73] Patients with oral lichen planus should be followed-up at least every 6 to 12 months, to assess the disease activity, changes in symptoms or even detect early signs of malignancy.
A similar variant of mucosal lichen planus as the vulvovaginal-gingival syndrome with erosive lesions involving oral and vulvovaginal mucosa were introduced by Pelisse and colleagues in year 1982.