mHealth
[7] Within the mHealth space, projects operate with a variety of objectives, including increased access to healthcare and health-related information (particularly for hard-to-reach populations); improved ability to diagnose and track diseases; timelier, more actionable public health information; and expanded access to ongoing medical education and training for health workers.
[9][page needed] A definition used at the 2010 mHealth Summit of the Foundation for the National Institutes of Health (FNIH) was "the delivery of healthcare services via mobile communication devices".
In many cases remote users are valuable contributors to gather data regarding disease and public health concerns such as outdoor pollution, drugs and violence.
In education and awareness applications, SMS messages are sent directly to users' phones to offer information about various subjects, including testing and treatment methods, availability of health services, and disease management.
These include phone consultations, counseling, service complaints, and information on facilities, drugs, equipment, and/or available mobile health clinics.
In such cases, known as telemedicine, patients might take a photograph of a wound or illness and allow a remote physician to diagnose to help treat the medical problem.
[16] Projects within this area operate to utilize mobile phones' ability to collect and transmit data quickly, cheaply, and relatively efficiently.
In the developing world, collecting field information is particularly difficult since many segments of the population are rarely able to visit a hospital, even in the case of severe illness.
[2] Within environments of limited resources and beds—and subsequently an 'outpatient' culture—remote monitoring allows healthcare workers to better track patient conditions, medication regimen adherence, and follow-up scheduling.
[17] Technical process evaluations have confirmed the feasibility of deploying dynamically tailored, SMS-based interventions designed to provide ongoing behavioral reinforcement for persons living with HIV.
[29] Possible organizational issues include the ensuring of appropriate use and proper care of the handset, lost or stolen phones, and the important consideration of costs related to the purchase of equipment.
[14] The use of mobile apps may sometimes lead to healthcare professionals spending more time performing additional tasks such as filling out electronic forms and may generate more workload in some cases.
[40] These countries face a severe lack of human and physical resources, as well as some of the largest burdens of disease, extreme poverty, and large population growth rates.
The WHO report findings also included that mHealth is most easily incorporated into processes and services that historically use voice communication through conventional telephone networks.
The report[42] was the result of a mHealth survey module designed by researchers at the Earth Institute's Center for Global Health and Economic Development,[43] Columbia University.
[3] Considering poor infrastructure and low human resources, the WHO notes that the healthcare workforce in sub-Saharan Africa would need to be scaled up by as much as 140% to attain international health development targets such as those in the Millennium Declaration.
[48] The WHO, in reference to the healthcare condition in sub-Saharan Africa, states: The problem is so serious that in many instances there is simply not enough human capacity even to absorb, deploy and efficiently use the substantial additional funds that are considered necessary to improve health in these countries.
[50] A progress report published in 2006 indicates that childhood immunization and deliveries by skilled birth attendants are on the rise, while many regions continue to struggle to achieve reductions in the prevalence of the diseases of poverty including malaria, HIV and AIDS and tuberculosis.
[52] Basic SMS functions and real-time voice communication serve as the backbone and the current most common use of mobile phone technology.
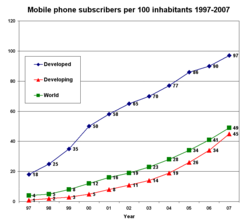
Improvements in telecommunications technology infrastructure, reduced costs of mobile handsets, and a general increase in non-food expenditure have influenced this trend.
[59] So, while mobile phones may have the potential to provide greater healthcare access to a larger portion of a population, there are certainly within-country equity issues to consider.
Although far from ubiquitous, the spread of smartphone technologies opens up doors for mHealth projects such as technology-based diagnosis support, remote diagnostics and telemedicine, preprogrammed daily self-assessment prompts, video or audio clips,[62] web browsing, GPS navigation, access to web-based patient information, post-visit patient surveillance, and decentralized health management information systems (HMIS).
[63] Beyond mobile phones, wireless-enabled laptops and specialized health-related software applications are currently being developed, tested, and marketed for use in the mHealth field.
However, with broad advocacy campaigns for free and open source software (FOSS), applications are beginning to be tailored for and make inroads in low- and middle-income countries.
This may foster greater adoption of mHealth technologies and services, by exploiting lower cost multi purpose mobile devices such as tablets, PCs, and smartphones.
Operating systems must be agile and evolve to effectively balance and deliver the desired level of service to an application and end user, while managing display real estate, power consumption and security posture.
With advances in capabilities such as integrating voice, video and Web 2.0 collaboration tools into mobile devices, significant benefits can be achieved in the delivery of health care services.
New sensor technologies[64] such as HD video and audio capabilities, accelerometers, GPS, ambient light detectors, barometers and gyroscopes[65] can enhance the methods of describing and studying cases, close to the patient or consumer of the health care service.
[57] With greater access to mobile phones to all segments of a country, including rural areas, the potential of lowering information and transaction costs in order to deliver healthcare improves.
The combination of these two factors has motivated much discussion of how greater access to mobile phone technology can be leveraged to mitigate the numerous pressures faced by developing countries' healthcare systems.