Maternal health
WHO has indicated that even though motherhood has been considered as a fulfilling natural experience that is emotional to the mother, a high percentage of women develop health problems, sometimes resulting in death.
"[10] In 2010 the U.S. Joint Commission on Accreditation of Healthcare Organizations described maternal mortality as a "sentinel event", and uses it to assess the quality of a health care system.
[12] Also, when women attend clinics without being charged and are issued with free supplements, their health is maintained, and this reduces the cost that the monetary resources that the government invests in healthcare.
Additionally, many approaches involving women, families, and local communities as active stakeholders in interventions and strategies to improve maternal health.
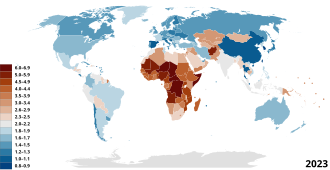
[citation needed] According to a UNFPA report, social and economic status, culture norms and values, and geographic remoteness all increase maternal mortality, and the risk for maternal death (during pregnancy or childbirth) in sub-Saharan Africa is 175 times higher than in developed countries, and risk for pregnancy-related illnesses and negative consequences after birth is even higher.
Throughout several studies, women and adolescents ranked inadequate finances and lack of transportation as the most common barriers to receiving proper prenatal care.
[32] Increased rates of hypertension, diabetes, respiratory complications, and infections are prevalent in cases of maternal obesity and can have detrimental effects on pregnancy outcomes.
[40][41]High intensity exercises such as stationary biking, uphill running, cross country skiing, and resistance circuit training, all showed similar benefits.
Maternal health organizations suggest that at a minimum pregnant women should receive one ultrasound at week 24 to help predict any possible growth anomalies and prevent future gestational concerns.
If their medical system is able to provide them, mothers can also undergo more invasive diagnostic tests such as an amniocentesis, or chorionic villous sampling to detect abnormalities with greater accuracy.
However, state specific reports show that Hispanic women still face high rates of maternal morbidity, or health problems that arise from pregnancy and birth.
[52] Black and Indigenous women can also encounter racial bias held by healthcare providers, which affects the quality of care given to treat or prevent a fatal disease.
For example, one such study stated that, due to the insensitivity and lack of knowledge that physicians showed immigrant Muslim women in Canada, their health information and treatment suffered.
[56] In order to provide a safer and more comfortable environment for Muslim women, it was proven that they needed more support that would connect with the immigrant community and health-related information.
[59] Future studies can look at how societal traditions or expectations such as gender roles may combine with religion to result in poorer maternal health care.
[citation needed] Although factors of religion can negatively influence maternal health care, other studies show the necessity of understanding different religious beliefs and practices.
[60] Spiritual interventions done by pastors in pregnancy included prayer, revelations, reversing negative dreams, laying of hands and anointing women.
[84] Excessive alcohol use during pregnancy can cause FASD, which commonly consist of physical and cognitive abnormalities in the child such as facial deformities, defective limbs, face, and heart, learning problems, below average intelligence, and intellectual disability (ID).
[89] Because the embryo or fetus's nutrition is based on maternal protein, vitamin, mineral, and total caloric intake, infants born to malnourished mothers are more likely to exhibit malformations.
[93] The majority of infants who contract HIV through breast milk do so within the first six weeks of life,[96] despite that antiretroviral treatment (during pregnancy, delivery and during breastfeeding) reduces transmission risk by >90%.
[43] Light exercise should be continued for pregnant mothers as it has been recommended to combat negative health outcomes, side effects and birth complications related to obesity.
"[10][119] The U.S. Joint Commission on Accreditation of Healthcare Organizations calls maternal mortality a "sentinel event", and uses it to assess the quality of a health care system.
[11] Maternal mortality data is said to be an important indicator of overall health system quality because pregnant women survive in sanitary, safe, well-staffed and stocked facilities.
"[128] According to the United States Centers for Disease Control and Prevention (CDC), c. 4 million women who give birth in the US annually, over 50,000 a year, experience "dangerous and even life-threatening complications.
The WHO estimates that the cost to provide basic family planning for both maternal and neonatal health care to women in developing countries is US$8 per person a year.
The United Nations Population Fund (UNPFA) recently began its Campaign on Accelerated Reduction of Maternal Mortality in Africa (CARMMA), focusing on providing quality healthcare to mothers.
[134] Improving maternal health is the fifth of the United Nations' eight Millennium Development Goals (MDGs), targeting a reduction in the number of women dying during pregnancy and childbirth by three quarters by 2015, notably by increasing the usage of skilled birth attendants, contraception and family planning.
[126] Increasing contraceptive usage and family planning also improves maternal health through reduction in numbers of higher risk pregnancies and by lowering the inter-pregnancy interval.
The government should invest in this operation as when the rate of underage, as well as unplanned pregnancies, are reduced the healthcare cost stand a chance to drop by up to 8%.
Third, emergency obstetric care to address the major causes of maternal death which are hemorrhage, sepsis, unsafe abortion, hypertensive disorders and obstructed labour.