Medicine
Medicine is the science[1] and practice[2] of caring for patients, managing the diagnosis, prognosis, prevention, treatment, palliation of their injury or disease, and promoting their health.
[9] In the developed world, evidence-based medicine is not universally used in clinical practice; for example, a 2007 survey of literature reviews found that about 49% of the interventions lacked sufficient evidence to support either benefit or harm.
Depending upon the health insurance plan and the managed care system, various forms of "utilization review", such as prior authorization of tests, may place barriers on accessing expensive services.
On subsequent visits, the process may be repeated in an abbreviated manner to obtain any new history, symptoms, physical findings, lab or imaging results, or specialist consultations.
From ancient times, Christian emphasis on practical charity gave rise to the development of systematic nursing and hospitals, and the Catholic Church today remains the largest non-government provider of medical services in the world.
Surgery is an ancient medical specialty that uses operative manual and instrumental techniques on a patient to investigate or treat a pathological condition such as disease or injury, to help improve bodily function or appearance or to repair unwanted ruptured areas (for example, a perforated ear drum).
[30] These terms, internist or physician (in the narrow sense, common outside North America), generally exclude practitioners of gynecology and obstetrics, pathology, psychiatry, and especially surgery and its subspecialities.
In North America, it requires at least three years of residency training after medical school, which can then be followed by a one- to three-year fellowship in the subspecialties listed above.
It typically involves entry level education at a university medical school, followed by a period of supervised practice or internship, or residency.
A database of objectives covering medical knowledge, as suggested by national societies across the United States, can be searched at http://data.medobjectives.marian.edu/ Archived 4 October 2018 at the Wayback Machine.
While the laws generally require medical doctors to be trained in "evidence based", Western, or Hippocratic Medicine, they are not intended to discourage different paradigms of health.
Doctors who are negligent or intentionally harmful in their care of patients can face charges of medical malpractice and be subject to civil, criminal, or professional sanctions.
As a scholarly discipline, medical ethics encompasses its practical application in clinical settings as well as work on its history, philosophy, theology, and sociology.
For example, some argue that the principles of autonomy and beneficence clash when patients refuse blood transfusions, considering them life-saving; and truth-telling was not emphasized to a large extent before the HIV era.
[37] In China, archaeological evidence of medicine in Chinese dates back to the Bronze Age Shang dynasty, based on seeds for herbalism and tools presumed to have been used for surgery.
Hippocrates introduced the Hippocratic Oath for physicians, which is still relevant and in use today, and was the first to categorize illnesses as acute, chronic, endemic and epidemic, and use terms such as, "exacerbation, relapse, resolution, crisis, paroxysm, peak, and convalescence".
[45][46] The Greek physician Galen was also one of the greatest surgeons of the ancient world and performed many audacious operations, including brain and eye surgeries.
[47] The concept of hospital as institution to offer medical care and possibility of a cure for the patients due to the ideals of Christian charity, rather than just merely a place to die, appeared in the Byzantine Empire.
[49] After 750 CE, the Muslim world had the works of Hippocrates, Galen and Sushruta translated into Arabic, and Islamic physicians engaged in some significant medical research.
[62][63] In Europe, Charlemagne decreed that a hospital should be attached to each cathedral and monastery and the historian Geoffrey Blainey likened the activities of the Catholic Church in health care during the Middle Ages to an early version of a welfare state: "It conducted hospitals for the old and orphanages for the young; hospices for the sick of all ages; places for the lepers; and hostels or inns where pilgrims could buy a cheap bed and meal".
The Schola Medica Salernitana in Salerno, looking to the learning of Greek and Arab physicians, grew to be the finest medical school in Medieval Europe.
The major shift in medical thinking was the gradual rejection, especially during the Black Death in the 14th and 15th centuries, of what may be called the "traditional authority" approach to science and medicine.
This was the notion that because some prominent person in the past said something must be so, then that was the way it was, and anything one observed to the contrary was an anomaly (which was paralleled by a similar shift in European society in general – see Copernicus's rejection of Ptolemy's theories on astronomy).
[67] Independently from Ibn al-Nafis, Michael Servetus rediscovered the pulmonary circulation, but this discovery did not reach the public because it was written down for the first time in the "Manuscript of Paris"[68] in 1546, and later published in the theological work for which he paid with his life in 1553.
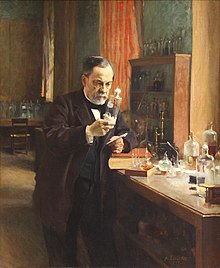
Modern scientific biomedical research (where results are testable and reproducible) began to replace early Western traditions based on herbalism, the Greek "four humours" and other such pre-modern notions.
From Germany and Austria, doctors Rudolf Virchow, Wilhelm Conrad Röntgen, Karl Landsteiner and Otto Loewi made notable contributions.
[71] Pharmacology developed in part from herbalism and some drugs are still derived from plants (atropine, ephedrine, warfarin, aspirin, digoxin, vinca alkaloids,[72] taxol, hyoscine, etc.).
Pharmacology has become increasingly sophisticated; modern biotechnology allows drugs targeted towards specific physiological processes to be developed, sometimes designed for compatibility with the body to reduce side-effects.
The movement is facilitated by modern global information science, which allows as much of the available evidence as possible to be collected and analyzed according to standard protocols that are then disseminated to healthcare providers.
These topics generate significant political and public policy attention, particularly in the United States where healthcare is regarded as excessively costly but population health metrics lag similar nations.