Methicillin-resistant Staphylococcus aureus
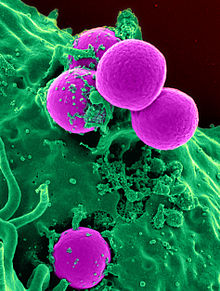
MRSA is any strain of S. aureus that has developed (through natural selection) or acquired (through horizontal gene transfer) a multiple drug resistance to beta-lactam antibiotics.
[citation needed] In humans, Staphylococcus aureus is part of the normal microbiota present in the upper respiratory tract,[2] and on skin and in the gut mucosa.
The initial presentation of MRSA is small red bumps that resemble pimples, spider bites, or boils; they may be accompanied by fever and, occasionally, rashes.
[13][26] Prisons and military barracks[19] can be crowded and confined, and poor hygiene conditions may proliferate, thus putting inhabitants at increased risk of contracting MRSA.
[31] Three studies by the Texas State Department of Health found the infection rate among football players was 16 times the national average.
[38] Children and adults who come in contact with day-care centers,[19] playgrounds, locker rooms, camps, dormitories, classrooms and other school settings, and gyms and workout facilities are at higher risk of contracting MRSA.
The unsanitary methods of injection causes an access point for the MRSA to enter the blood stream and begin infecting the host.
Furthermore, with MRSA's high contagion rate,[11] a common risk factor is individuals who are in constant contact with someone who has injected drugs in the past year.
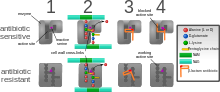
[41] A defining characteristic of MRSA is its ability to thrive in the presence of penicillin-like antibiotics, which normally prevent bacterial growth by inhibiting synthesis of cell wall material.
This is due to a resistance gene, mecA, which stops β-lactam antibiotics from inactivating the enzymes (transpeptidases) critical for cell wall synthesis.
[42] Staphylococcal cassette chromosome mec (SCCmec) is a genomic island of unknown origin containing the antibiotic resistance gene mecA.
[41] Owing to the size of the SCCmec element and the constraints of horizontal gene transfer, a minimum of five clones are thought to be responsible for the spread of MRSA infections, with clonal complex (CC) 8 most prevalent.
[50] In contrast, CA-MRSA tends to carry lower-fitness cost SCCmec elements to offset the increased virulence and toxicity expression required to infect healthy hosts.
[53] SpeG-positive ACME compensates for the polyamine hypersensitivity of S. aureus and facilitates stable skin colonization, wound infection, and person-to-person transmission.
[56] EMRSA16 has been found to be identical to the ST36:USA200 strain, which circulates in the United States, and to carry the SCCmec type II, enterotoxin A and toxic shock syndrome toxin 1 genes.
[55] In the United States, most cases of CA-MRSA are caused by a CC8 strain designated ST8:USA300, which carries SCCmec type IV, Panton–Valentine leukocidin, PSM-alpha and enterotoxins Q and K,[57] and ST1:USA400.
Normally, a bacterium must be cultured from blood, urine, sputum, or other body-fluid samples, and in sufficient quantities to perform confirmatory tests early-on.
[77] To prevent the spread of staphylococci or MRSA in the workplace, employers are encouraged to make available adequate facilities that support good hygiene.
[76] To prevent the spread of MRSA in the home, health departments recommend laundering materials that have come into contact with infected persons separately and with a dilute bleach solution; to reduce the bacterial load in one's nose and skin; and to clean and disinfect those things in the house that people regularly touch, such as sinks, tubs, kitchen counters, cell phones, light switches, doorknobs, phones, toilets, and computer keyboards.
[12][25] Mathematical models describe one way in which a loss of infection control can occur after measures for screening and isolation seem to be effective for years, as happened in the UK.
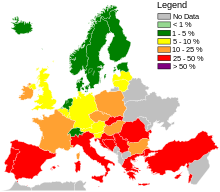
[80] One of the few countries not to have been overwhelmed by MRSA is the Netherlands: an important part of the success of the Dutch strategy may have been to attempt eradication of carriage upon discharge from hospital.
In the United Kingdom, the Workplace (Health, Safety and Welfare) Regulations 1992[84] require businesses to provide toilets for their employees, along with washing facilities including soap or other suitable means of cleaning.
CA-MRSA has a greater spectrum of antimicrobial susceptibility to sulfa drugs (like co-trimoxazole (trimethoprim/sulfamethoxazole), tetracyclines (like doxycycline and minocycline) and clindamycin (for osteomyelitis).
[4] Ceftaroline, a fifth-generation cephalosporin, is the first beta-lactam antibiotic approved in the US to treat MRSA infections in skin and soft tissue or community-acquired pneumonia.
[89] The Centers for Disease Control and Prevention (CDC) estimated that about 1.7 million nosocomial infections occurred in the United States in 2002, with 99,000 associated deaths.
(BMJ 2007)[citation needed] MRSA alone was associated with 8% of nosocomial infections reported to the CDC National Healthcare Safety Network from January 2006 to October 2007.
[19] In 1961, the first known MRSA isolates were reported in a British study, and from 1961 to 1967, infrequent hospital outbreaks occurred in Western Europe and Australia,[17] with methicillin then being licensed in England to treat resistant infections.
[146][147] Host-directed therapeutics, including host kinase inhibitors, as well as antimicrobial peptides are under study as adjunctive or alternative treatment for MRSA.
[148][149][150] A 2015 Cochrane systematic review aimed to assess the effectiveness of wearing gloves, gowns and masks to help stop the spread of MRSA in hospitals, however no eligible studies were identified for inclusion.
The review authors concluded that there is a need for randomized controlled trials to be conducted to help determine if the use of gloves, gowns, and masks reduces the transmission of MRSA in hospitals.