Modes of mechanical ventilation
[1] There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups.
[2][3] Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy (i.e. PC-IMV, or VC-MMV etc.).
In other words, the right hand side of the equation of motion remains constant while pressure changes with changes in elastance and resistance.Pressure control (PC) means that inspiratory pressure is preset as either a constant value or it is proportional to the patient's inspiratory effort.
In other words, the left-hand side of the equation of motion remains constant while volume and flow change with changes in elastance and resistance.Time control (TC) means that, in some rare situations, none of the main variables (pressure, volume, or flow) are preset.
The targeting schemes can be represented by single, lower case letters: set-point = s, dual = d, servo = r, bio-variable = b, adaptive = a, optimal = o, intelligent = i.
While 'APRV' is common to users in North America, a very similar mode, biphasic positive airway pressure (BIPAP), was introduced in Europe.
[7] The term APRV has also been used in American journals where, from the ventilation characteristics, BIPAP would have been perfectly good terminology.
Although similar in modality, these terms describe how a mode is intended to inflate the lung, rather than defining the characteristics of synchronization or the way spontaneous breathing efforts are supported.
Since the American Association for Respiratory Care established a nomenclature of mechanical ventilation the "synchronized" part of the title has been dropped and now there is only IMV.
[citation needed] MMV is an optimal mode for weaning in neonatal and pediatric populations and has been shown to reduce long-term complications related to mechanical ventilation.
Pressure-regulated volume control utilizes pressure-limited, volume-targeted, time-cycled breaths that can be either ventilator- or patient-initiated.
The peak inspiratory pressure delivered by the ventilator is varied on a breath-to-breath basis to achieve a target tidal volume that is set by the clinician.
Automatic positive airway pressure (APAP) is a form of CPAP that automatically tunes the amount of pressure delivered to the patient to the minimum required to maintain an unobstructed airway on a breath-by-breath basis by measuring the resistance in the patient's breathing.
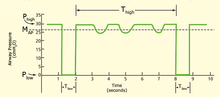
BPAP can be described as a Continuous Positive Airway Pressure system with a time-cycle change of the applied CPAP level.
[11] CPAP/APAP, BPAP, and other non-invasive ventilation modes have been shown to be effective management tools for chronic obstructive pulmonary disease, acute respiratory failure, sleep apnea, etc.
With HFPV it utilizes an open circuit to deliver its subtidal volumes by way of the patient interface known as the Phasitron.
PEEP is a pressure that an exhalation has to bypass, in effect causing alveoli to remain open and not fully deflate.
[20] Negative-pressure ventilation stimulates (or forces) breathing by periodic application of partial vacuum (air pressure reduced below ambient pressure), applied externally to the patient's torso—specifically, chest and abdomen—to assist (or force) the chest to expand, expanding the lungs, resulting in voluntary (or involuntary) inhalation through the patient's airway.
[33][34][35][36][37] Various "negative pressure ventilators" (NPVs) have been developed to serve this function—most famously the "Iron lung," a tank in which the patient lays, with only their head exposed to ambient air, while air pressure on the remainder of their body, inside the tank, is varied by pumping, to stimulate chest and lung expansion and contraction.
In terms of patient-ventilator synchrony, NAVA supports both resistive and elastic work of breathing in proportion to the patient's inspiratory effort Proportional assist ventilation (PAV) is another servo targeting based mode in which the ventilator guarantees the percentage of work regardless of changes in pulmonary compliance and resistance.
PAV, like NAVA, supports both restrictive and elastic work of breathing in proportion to the patient's inspiratory effort.
The use of perfluorochemicals, rather than nitrogen, as the inert carrier of oxygen and carbon dioxide offers a number of theoretical advantages for the treatment of acute lung injury, including: Despite its theoretical advantages, efficacy studies have been disappointing and the optimal clinical use of LV has yet to be defined.