Neonatal meningitis
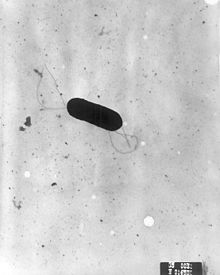
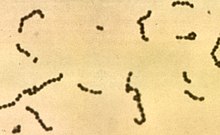
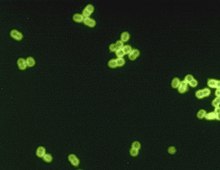
Organisms responsible are different; most commonly group B streptococci (i.e. Streptococcus agalactiae), Escherichia coli, and Listeria monocytogenes.
[1] Delayed treatment of neonatal meningitis may cause cerebral palsy, blindness, deafness, seizure disorders, and learning deficiencies.
Complications should be suspected when the clinical course is characterized by shock, respiratory failure, focal neurological deficits, a positive cerebrospinal fluid culture after 48 to 72 hours of appropriate antibiotic therapy, or infection with certain organisms, such as Citrobacter koseri and Cronobacter sakazakii for example.
Children are assessed through behavioral testing (if old enough), Otoacoustic Emissions (OAEs), and Auditory Brainstem Response (ABR).
[citation needed] Impact in Children for Communication If hearing loss is left undetected and/or untreated, this can lead to later acquisition of language and delayed reading skills.
[16] [17] Even more rare, Meningitis can be caused by some cancers, Lupus, specific drugs, head injuries, and brain surgeries.
[18] Most neonatal meningitis results from bacteremia (bacterial infection of the blood) with hematogenous spread to the central nervous system (CNS).
In developing countries, Gram-negative enteric (gut) bacteria are responsible for the majority of early onset meningitis.
The bacteria then invades through the intestinal mucosa layer into the blood, causing bacteremia followed by invasion of the cerebrospinal fluid.
Evidence suggests that vaginal colonization by Streptococcus agalactiae during pregnancy increases the risk of vertical transmission and early-onset disease in neonates.
Cerebrospinal fluid culture is the most important study for the diagnosis of neonatal bacterial meningitis because clinical signs are non-specific and unreliable.
The role of the spinal tap in neonates who are healthy appearing but have maternal risk factors for sepsis is more controversial; its diagnostic yield in these patients may be low.
[19] Samples should be taken from skin, conjunctiva (eye), mouth and throat, rectum, urine, and the cerebrospinal fluid for viral culture and polymerase chain reaction.
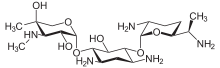
The particular drugs used are based on culture results that identify the infecting bacteria, but a mix of ampicillin, gentamicin, and cefotaxime is used for early-onset meningitis before their identification.
A regimen of antistaphylococcal antibiotic, such as nafcillin or vancomycin, plus cefotaxime or ceftazidime with or without an aminoglycoside is recommended for late-onset neonatal meningitis.
[1][6] For suspected Gram-negative enteric (including E. coli) meningitis a combination of cefotaxime and aminoglycoside, usually gentamicin, is recommended.
[1][6] Meningitis caused by Listeria monocytogenes should be treated with a combination of ampicillin and gentamicin because it is synergistic in vitro and provides more rapid bacterial clearance in animal models of infection.
[1][6] In cases of meningitis caused by Herpes simplex virus, antiviral therapy with (acyclovir or vidarabine) must be started immediately for a favorable outcome.
It is expected that these numbers are lower than reality due to the difficulty of diagnosing and the healthcare available to underdeveloped countries in Asia and Africa.